第十二届全国癌症康复与姑息医学大会:阿片类药物的合理应用
2016-06-23 MedSci MedSci原创
2016年6月17日~19日,第十二届全国癌症康复与姑息医学大会在合肥盛大举行。大会主席王杰军教授指出,国内一直存在姑息治疗的理念,但没有得到规范化的实施。CRPC委员会首先从肿瘤疼痛的规范化治疗做起。在此次会议中,由CRPC联合萌蒂制药公司启动了“2016-2018癌痛规范化全程管理项目”,投入1000万人民币的项目,为进一步加强中国癌痛病人的规范化管理,此项目必将为减少肿瘤患者的癌痛带来真
2016年6月17日~19日,第十二届全国癌症康复与姑息医学大会在合肥盛大举行。
大会主席王杰军教授指出,国内一直存在姑息治疗的理念,但没有得到规范化的实施。CRPC委员会首先从肿瘤疼痛的规范化治疗做起。在此次会议中,由CRPC联合萌蒂制药公司启动了“2016-2018癌痛规范化全程管理项目”,投入1000万人民币的项目,为进一步加强中国癌痛病人的规范化管理,此项目必将为减少肿瘤患者的癌痛带来真切的益处,开启中国肿瘤姑息治疗的新篇章!
会议中,浙江省肿瘤医院化疗中心张沂平主任指出,中国在80个国家的综合排名中位列第71位,这反映出姑息治疗总体的供应有限,而且质量不高。在中国,中度癌痛患者比例高,强阿片类药物治疗不足,癌痛患者中6成为中度癌痛,中度癌痛患者不足2成使用强阿片类药物。我们的人口占世界的20%,但阿片类药物使用只占2%,我国的大部分癌症患者仍受着癌痛的折磨,未来中国的姑息治疗仍有很多工作要做。
拥有较高的死亡质量的国家有一些共同特点
强大且得到有效实施的国家姑息治疗政策框架
在医疗保健服务方面保持高水平的公共开支
为普通和专业医疗工作者提供广泛的姑息治疗培训资源
提供慷慨的补贴,以减轻病人接受姑息治疗的财务负担
阿片类镇痛剂的广泛供应
公众对姑息治疗的高度认识
2014年JCO发表的一篇文章中,提出癌痛管理的障碍:
疼痛评估不足
知识缺乏
不愿处方阿片类药物
担心不良反应
担心耐受性
担心药物成瘾
担心法律限制
担心法律限制
政府当局的过度管控
认为吗啡在大众观念中是负面的
护士不愿意护理
医护人员对自己的知识水平过高的评估
……
由上可知,中国在癌痛管理和阿片类药物使用规范和普及上依然任重道远。
之后,北大肿瘤国际医院部常务梁军主任作了“阿片类药物合理应用”讲题,梅斯医学小编整理如下:
梁军教授:阿片类药物的合理应用
癌痛产生的影响是一个恶性循环的过程,在身体上,会引起食欲不振、营养不良、睡眠障碍,消瘦,工作能力下降或丧失,活动能力下降,免疫力低下,易感染,疾病进展。
在心理上,患者会对药物产生依赖感,对家人过度依赖,丧失尊严;疼痛导致焦虑等负性情绪使痛痛域下降。疼痛导致对肿瘤的过度医疗。浪费医疗资源。
然而,癌痛尚未得到足够的治疗。
癌痛是全球的健康问题,每年500余万晚期癌症患者遭受癌痛的折磨,但是癌痛控制不佳。
癌痛控制是姑息治疗的重要组成部分。癌痛治疗使肿瘤患者获益,可增强患者信心,提高对肿瘤治疗的顺应性,患者生活质量迅速得到改善,使肿瘤治疗的结局更好。
阿片类药物是中重度癌痛的一线药物,合理使用尤为重要,合理应用包括:“合适的药物、合适的剂量、用于合适的患者。”
然而,合理选择阿片类药物仍存在问题。主要包括药物选择,给药途径,给药剂量,给药时机。
梁军教授主要从癌症疼痛治疗原则,阿片类药物的合理选择,强阿片药物相关临床研究三个方面进行介绍。
1986年WHO提出的癌痛三阶梯指导原则依旧使用至今,包括首选口服,按时给药,按阶梯给药,个体化治疗,注重细节等内容。
首选口服给药的优点:简单、经济,易于接受,血药浓度稳定,与静脉注射同样有效,剂量调整方便,更有自主性,不易成瘾及产生耐药性。
按时给药:按照规定时间间隔给药,如每隔12小时一次,无论给药当时病人是否发作疼痛,而非按需给药,这样可保证疼痛连续缓解。
合适的剂量定义为:缓解疼痛、最大程度的改善患者功能,不造成无法处理的副作用。
个体化给药:对麻醉药品的敏感度个体间差异很大,因此阿片类药物并没有标准量。
注意具体细节:对用止痛药的患者要注意监护,密切观察其反应,目的是使患者获得最佳疗效,而发生的副作用却最小,提高患者生活质量。
癌痛治疗药物种类繁多,合理选择是关键。
药物包括:(图1)
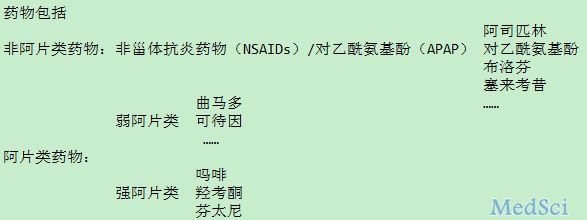
图1
非甾体抗炎药物(NSAIDs)对乙酰氨基酚(APAP)可用于轻度疼痛
使用注意事项:
剂量限制:
对乙酰氨基酚,在肝功能正常的成人患者,650mg/4小时/次,或1g/6小时/次(每日最高剂量4g/d)。由于肝脏毒性,对于长期服用对乙酰氨基酚的患者,日剂量上限为3g/d或更低。
副作用:
1.慎用NSAIDs,尤其是长期服用患者,许多肿瘤患者是肾脏,消化道(上消化道手术、放疗)、心脏毒性,血小板减少症,出血性疾病的高危人群。注意化疗的潜在不良反应如血液、肾脏、肝脏和心血管系统毒性,可随着同时使用NSAIDs而增加。
2、考虑到存在肝脏毒性,为了避免对乙酰氨基酚过量,应慎用对乙酰氨基酚,或不使用对乙酰氨基酚复方制剂。
如果需要长期使用NSAIDs或日用剂量已达到限制性用量时,应考虑更换为阿片类止痛药;如为联合用药,则只增加阿片类止痛药用药剂量。
WHO三阶梯止痛原则的变迁
WHO三阶梯止痛原则虽然使用至今,但随着临床发展,有人提出疑问:二阶梯药物是否仍必要?
强阿片类药物用于中度癌痛—临床研究证据
l强阿片类药物用于中度疼痛,疗效佳,换药少。
l一阶梯后直接起始羟考酮缓释片获得有效镇痛
l对于中度癌痛患者,低剂量吗啡对疼痛控制相较于弱阿片类有更好的疗效和更好的耐受性。
低剂量阿片类药物治疗中度疼痛证据
l疼痛评分≥4分可以选择强阿片类药物
l2016年NCCN成人癌痛指南指出:疼痛评分≥4分(中重度疼痛),建议吗啡滴定
l2012年EAPC指南指出:低剂量第三阶梯药物(如吗啡或羟考酮)可作为第二阶段(如可待因或曲马多)的替代药物
l2012年ESMO癌痛管理临床实践指南中指出:考虑低剂量的强阿片类药物联合非阿片类镇痛药作为弱阿片类药物的替代药物。
合理的阿片类药物选择
合理选择阿片类药物很关键,需考虑以下因素:
疾病情况
疼痛程度
疼痛特点
药物特点
阿片类药物分类(图2)
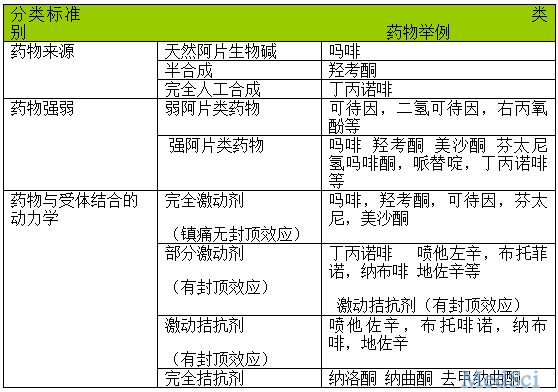
图2
弱阿片类药物——可用于中度疼痛
曲马多
l具有阿片受体激动和脊髓去甲肾上腺与5-羟色胺摄取抑制双重作用,影响痛觉传导产生镇痛作用
l镇痛强度是吗啡的1/10
l每日最大剂量400mg
l使用曲马多时,应慎用或避免使用作用于5-羟色胺能神经元或单胺氧化酶抑制剂等药物,防止出现5-羟色胺综合征。
强阿片类药物——可用于中重度疼痛
常见的三种强阿片类药物比较(图3)
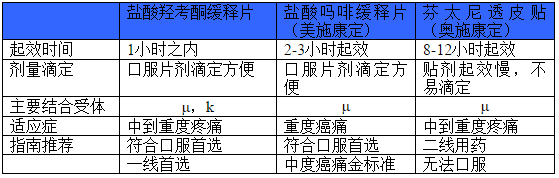
图3
羟考酮与阿片受体作用特点(图4)
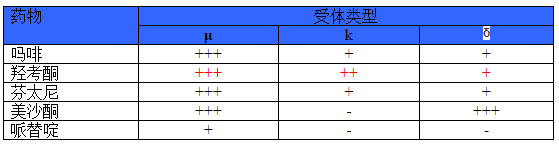
图4
l与吗啡,芬太尼相比,羟考酮对K手提亲和力更强,而k受体与内脏痛,神经病理性疼痛相关
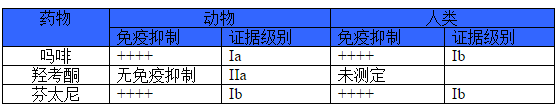
不同阿片药物的免疫抑制作用
l强阿片类药物能够有效控制疼痛,减少应激,但也有文献记录部分阿片药物本身会影响免疫系统功能
l研究总结了不同的阿片类药物用于动物和人体的免疫抑制作用。(图5)
强阿片类药物使用注意事项(NCCN指南建议):
芬太尼贴剂:
芬太尼透皮贴在使用前,应当先进行短小阿片药物的滴定直至疼痛良好控制。
贴剂不推荐用于需药频繁调整剂量的不稳定疼痛患者,应当用于阿片耐受患者
避免芬太尼贴剂使用的部位和周边暴露在热源下。温度升高使芬太尼释放激素,会导致剂量过量和死亡。
芬太尼贴剂不能剪开或刺破
不推荐用于癌痛治疗的药物
哌替啶
混合激动——拮抗剂(如地佐辛)
强阿片药物治疗癌痛相关研究
临床上,需结合患者疾病特点,疼痛程度,性质,选择合适的阿片类药物。
基于不同人群的临床研究,为合理选择阿片类药物提供了证据支持。
强阿片药物治疗癌痛相关研究包括内脏痛、躯体痛、神经病理痛、门诊与院外应用及合理剂量的探索。
一、2010年发表在european review for medical and pharmacological sciences的一篇前瞻性,多中心,随机观察性研究,探究了盐酸羟考酮缓释片治疗癌性内脏痛的效果。(2010;14;185-190)
研究对象:年龄≥18岁,疼痛未控制且NRS评分≥4分的976例患者。使用奥施康定治疗15天,每个患者初始计量个体化。研究重点是疼痛强度(NRS)、生活质量评价(SF-12)及不良事件。结果显示治疗后疼痛程度显著降低,基线时严重疼痛患者为67.7%,15天后降低为1.5%;重度不良事件发生率低。
二、2009年发表在European Neurology上一篇意大利多中心研究:评估盐酸羟考酮缓释片联合普瑞巴林对于神经病理性疼痛的疗效与安全性。(2009;61::19-137)入选409例中至重度神经性病理疼痛患者。
研究分组:
普瑞巴林组(n=134,起始剂量85.6mg/天)
盐酸羟考酮缓释片(n=106,起始剂量24.1mg/天)
盐酸羟考酮缓释片+普瑞巴林(n=169,起始剂量分别是19.4mg/天)。
治疗时间:90天
主要终点:疼痛缓解(NRS评分)
结果:与基线相比,治疗90天后治疗组患者疼痛评分下降比率:
联合治疗组:80%
盐酸羟考酮缓释片治疗组:76%
普瑞巴林治疗组:46%
联合用药组与两个单药组比较,差异有统计学意义。
联合用药或单用盐酸羟考酮缓释片组——更快速且更强效缓解患者疼痛,显著降低患者爆发痛平均发生次数。
考虑:各治疗组患者不良反应发生情况
与单药治疗相比,盐酸羟考酮缓释片与普瑞巴林联合治疗降低了患者的不良反应。
三、2013年发表在Pain Medcine上的门诊癌症患者使用羟考酮缓释片进行疼痛的一项前瞻性非干预观察性研究。(2013 Dec:14(12):1866-72)对486名癌痛患者进行8周时间的研究,研究终点为疼痛评分、生活质量。研究结果显示门诊癌痛患者合理剂量使用羟考酮缓释片进行患者疼痛治疗是安全、有效、可耐受的。
小结:
癌痛治疗过程中,根据患者疾病预癌痛的不同特点,合理选择阿片类药物很关键。
合理使用阿片类药物定义为
有效镇痛
副作用可耐受
最大限度改善患者功能
更多精彩内容,请关注梅斯医学APP

小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#第十二届#
42
#合理应用#
44
文章不错,值得拜读
74
文章不错,值得拜读
81
#阿片类药物#
40
#阿片类#
23
#姑息#
41