JACC:血中酮体不仅会导致酮症,居然还会影响心肌梗死结局!
2021-09-30 MedSci原创 MedSci原创
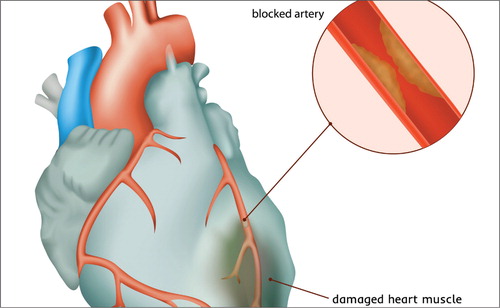
心肌梗死(MI)仍然是心力衰竭(HF)发展的一个主要风险因素。
尽管过去几十年来死亡率和发病率不断下降,但心肌梗死(MI)仍然是心力衰竭(HF)发展的一个主要风险因素。HF的心肌代谢已被发现依赖于酮体(KBs)作为主要的细胞能量来源,参与KB氧化的酶相应上调,循环中的KB水平增加。
HF中血浆KBs的上调被认为是由神经激素因素如儿茶酚胺和钠尿肽的上调引起的肝脏生酮作用增加的结果。儿茶酚胺和钠尿肽都会刺激脂肪细胞的脂肪分解,并促进非酯化脂肪酸的释放,而非酯化脂肪酸是生酮的重要代谢前体。
然而,循环中的KBs在缺血/再灌注中的作用仍然未知。为了调查ST段抬高型心肌梗死(STEMI)患者的KBs的纵向变化及其与功能结局的关系,来自荷兰格罗宁根大学心血管病的专家开展了相关研究,结果发表在JACC杂志上。

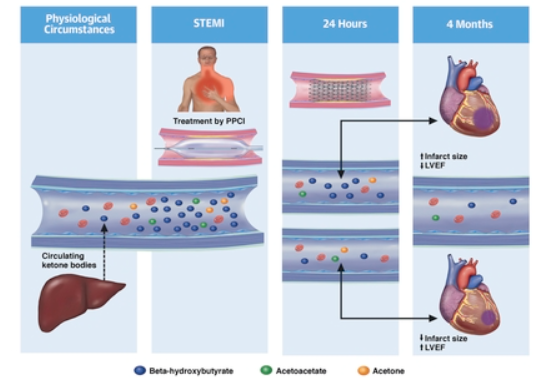
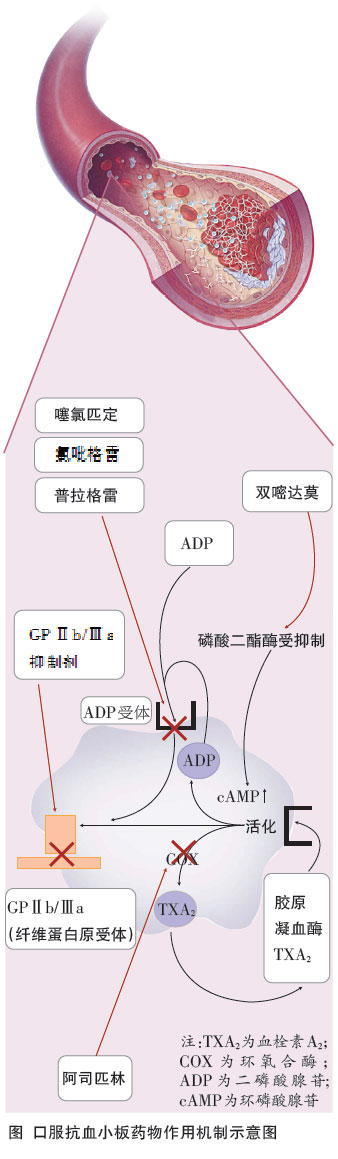
研究人员对来自STEMI后早期二甲双胍治疗随机试验的369名参与者进行KBs测量。在发病时、24小时后和4个月后,通过核磁共振光谱仪测量KBs(β-羟基丁酸、乙酰乙酸和丙酮)的非空腹血浆浓度。4个月后通过心脏磁共振成像确定心肌梗死的大小和左心室射血分数(LVEF)。使用多变量线性回归分析确定循环中的KBs与心肌梗死大小和左心室射血分数的关系。
结果显示,循环KBs在STEMI发病时很高(总KBs中位数:520 μmol/L;四分位数范围[IQR]:315-997 μmol/L)。再灌注后24小时,与4个月的随访水平相比,KBs仍然很高(分别为206 μmol/L [IQR: 174-246] vs 166 μmol/L [IQR: 143-201])。24小时内KB浓度的增加与心肌梗死面积的增大(总KBs,每100μmol/L:β = 1.56;95%置信区间:0.29-2.83)和LVEF的降低(β = -1.78;95%CI:(-3.17至-0.39)独立相关。
急性NSTEMI后血中酮体水平及其对预后的关系
综上,循环中的KBs在出现STEMI的患者中增加。24小时内较高的KBs与STEMI后的功能结果有关,这表明酮类代谢在应对心肌缺血中的潜在作用。
参考文献:
Association of Circulating Ketone Bodies With Functional Outcomes After ST-Segment Elevation Myocardial Infarction. J Am Coll Cardiol. 2021 Oct, 78 (14) 1421–1432
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JACC#
47
#酮症#
49
#学习#
45
#ACC#
35
谢谢分享
68