Nature reviews:肠上皮细胞死亡及其与慢性炎症的关系
2020-07-28 佚名 免疫细胞研究bioworld
综述了肠道疾病中IECs中控制程序性细胞死亡的分子和细胞基础,还讨论了细胞死亡调节的翻译方面,以开发用于炎症性肠病和大肠癌的新型治疗替代方法。
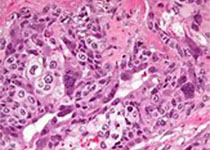
肠上皮细胞是细胞更替率最高的细胞之一,这一过程受到严格的调控。由于肠上皮的传递-放大祖细胞每天每个隐窝生成约300个细胞,调节根底表面的细胞死亡和脱落使细胞总数得到控制。肠上皮细胞(IEC)的异常增长是广泛的上皮糜烂的基础,这是一些肠道疾病的特征,如炎症性肠病和感染性结肠炎。新出现的证据指出,除了细胞凋亡以外,坏死、自噬和焦亡是小肠细胞程序性死亡的重要模式。细胞死亡模式影响组织恢复反应,并最终影响肠纤维化和结直肠癌的长期风险。肠道屏障的破坏、细胞的非正常死亡和随后的炎症是慢性炎症和感染性胃肠疾病的核心。本文综述了肠道疾病中IECs中控制程序性细胞死亡的分子和细胞基础,还讨论了细胞死亡调节的翻译方面,以开发用于炎症性肠病和大肠癌的新型治疗替代方法。
Key points
1. 在炎症性肠病患者的肠道活跃发作期间,各种程序性细胞死亡模式升高,损害肠道屏障
2. 肠上皮细胞发生程序性细胞死亡的模式有缺失、凋亡、坏死和焦亡等
3. 细胞坏死和焦亡是促炎作用,导致炎症的扩散,而anoikis和凋亡抑制炎症的扩散
4. GSDMD和MLKL是两种宿主蛋白,分别通过膜孔的形成导致细胞内内容物渗漏和细胞死亡。
5. 根据细胞死亡的模式,来自死亡细胞的因子可以触发代偿性增殖,以取代炎症过程中失去的细胞
6. 目前迫切需要确定炎症性肠病患者肠道不同细胞间不同类型细胞死亡的比例
肠上皮细胞死亡模式
在过去的几年中,我们对IEC中调节性细胞死亡机制的理解已迅速改变。除了确定影响IEC的多种细胞死亡模式外,对这些途径的建模和各种介体的作用也在不断修订中。例如,1997年发现了EGF信号对IECs的抗凋亡作用,但直到2017年才发现EGF信号通过mapk依赖途径对caspase依赖和caspase不依赖的IEC挤压和脱落的作用。不同类型的IEC对不同模式的细胞死亡的易感性很可能存在内在的差异。一项研究强调了septin亚型ARTS在小鼠和人LGR5+干细胞和Paneth细胞中高表达的促凋亡作用。也有证据表明干细胞坏死细胞死亡,触发事件的基因组不稳定是由转录活性的逆转录转座子在宿主细胞基因组。其他研究表明,Paneth细胞在被免疫细胞来源的IFN就绪触发时,会发生细胞挤压,而在没有caspase 8的情况下,它们会发生坏死细胞死亡。
细胞凋亡、坏死及对屏障功能的影响
与大多数其他细胞类型一样,IEC细胞凋亡被认为是免疫沉默的。巨噬细胞吞噬凋亡细胞通过自分泌或旁分泌因子如肝细胞生长因子(HGF)和PGE2启动愈合反应。因此,经典的细胞凋亡是抑制肠道进一步炎症的重要过程。诱导外源性受体驱动的IEC凋亡的途径成分,如启动子和效应子caspases、FADD和TNF受体,以及内在线粒体驱动的IEC凋亡,如Bcl-xL、Bcl-2和细胞色素c,在其他细胞类型中也很常见。尽管对凋亡进行了细致的分类,以区别于其他细胞死亡模式,但新的证据表明,线粒体驱动的内在凋亡和坏死之间存在大量的串扰,坏死通常被认为是一种免疫原性的细胞死亡形式。例如,在人细胞系中发现坏死通路的关键成分RIPK3和MLKL可以介导Bcl-2家族蛋白、内源性凋亡的重要介质PUMA的转录。另一项研究还发现,在肠道损伤RIPK3监管NF-κB-mediated细胞因子的生产和组织修复,这是经典与necroptosis无关。
细胞异常死亡的后果
细胞凋亡是一种免疫沉默形式的细胞死亡,而焦亡和坏死的IECs主要是溶解,促炎模式的细胞死亡,进一步组织损伤。这种差异主要是由于凋亡小体的形成阻止了损伤相关分子模式(DAMPs)的裂解扩散。凋亡效应因子,caspase介导的蛋白水解也使一些促炎细胞因子失活。通常,IECs的死亡导致他们从上皮单层挤压。当死亡的肠上皮细胞经历动态的微管重构时,邻近的上皮细胞响应并重组自己的细胞骨架网络,创造一个多细胞交界处,并将死亡细胞推出肠腔,同时保持上皮细胞的连续性。这一过程是IEC死亡的一个特征,有报道显示管腔小泡中有坏死或凋亡的小体脱落。这个过程有两个目的:被感染的IECs被移到富含抗菌剂和粘液的腔内,阻止死亡细胞内的病原体进入粘膜下;死细胞释放到粘膜下的炎性湿气的负荷被最小化,从而阻止了免疫系统的全面激活。
总结
在过去的5 - 10年里,对肠内细胞死亡程序的研究大大提高了我们对IBD过程和生物学的理解。然而,在未来,我们还需要对IBD具体病例中特定细胞死亡途径的治疗靶点有更深入的了解。持续的肠道屏障功能障碍、微生物异常、IEC死亡和炎症是IBD的特征。在某些条件下,IECs更容易因炎症驱动的作用而死亡,从而导致进一步的屏障破坏和生态失调。IBD的最终治疗目标是通过抑制IEC死亡和促进炎症的持续解决来防止肠道屏障的破坏。细胞凋亡的增加和IECs的坏死现在被确定与IBD的炎症严重程度有关。在IBD的临床前模型中,对IEC死亡的遗传和药理学抑制能够恢复屏障功能。然而,由于潜在的不利副作用,如抑制活化T细胞的细胞死亡或触发潜在的致癌旁观者,直接针对IEC死亡的治疗方法存在怀疑。然而,未来对细胞类型特异性细胞死亡机制的研究将有助于更好地了解IBD的新治疗方法。
原始出处:
Jay V Patankar, Christoph Becker.Cell death in the gut epithelium and implications for chronic inflammation.Review Nat Rev Gastroenterol Hepatol. 2020 Jul 10. doi: 10.1038/s41575-020-0326-4..
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#review#
48
#肠上皮细胞#
52
学习了
108
#Nat#
45
#reviews#
52
#上皮细胞#
54