Nature Commun:小分子可促进缓解心脏衰竭
2015-06-17 佚名 生物谷
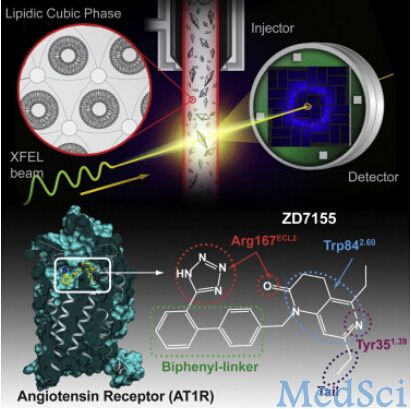
在心脏细胞中,心肌肌质网的钙离子相关的ATP合成酶(SERCA2a)的表达和活性的降低,被认为是心脏衰竭的标志。这个酶(SERCA2a)是一个与钙离子循环相关的关键性转运离子泵。之前他们发现了一种转录后修饰,即可反转的SUMO化修饰(类似于泛素化修饰),可以调节酶SERCA2a的功能进而影响心脏的功能。这种SUMO修饰可能在多方面影响着细胞的功能。就这个酶SERCA2a而言,存在着多种小的SUMO
在心脏细胞中,心肌肌质网的钙离子相关的ATP合成酶(SERCA2a)的表达和活性的降低,被认为是心脏衰竭的标志。这个酶(SERCA2a)是一个与钙离子循环相关的关键性转运离子泵。之前他们发现了一种转录后修饰,即可反转的SUMO化修饰(类似于泛素化修饰),可以调节酶SERCA2a的功能进而影响心脏的功能。这种SUMO修饰可能在多方面影响着细胞的功能。就这个酶SERCA2a而言,存在着多种小的SUMO修饰因子。例如,早期的研究表明,在啮齿动物和其他大型动物的模型上,心脏衰竭可能通过转入一种这样的SUMO修饰因子SUMO-1基因,可以恢复心脏的功能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#COMMUN#
33
是一篇不错的文章
122
这篇文章有一定深度
131
关注小分子
123
#Nat#
34
#小分子#
26
看看
158
多学习前沿,进步
152
期待更多研究
45
早日进入临床试验
86