Circulation:依洛尤单抗长期治疗对已知动脉粥样硬化性心血管疾病的疗效
2022-08-30 MedSci原创 MedSci原创
长期使用依洛尤单抗降低LDL-C与持续较低的不良事件发生率相关。
在FOURIER试验中,PCSK9抑制剂依洛尤单抗降低了LDL-C和心血管事件的风险,并且在2.2年的中位随访中是安全且耐受性良好的。然而,缺乏大规模、长期的数据。

近日,心血管领域权威杂志Circulation上发表了一篇研究文章,研究人员将27564名LDL-C≥70mg/dl的ASCVD患者随机分为依洛尤单抗组和安慰剂组。
该研究的主要分析汇集了各个研究,主要终点是不良事件的发生率。研究人员前瞻性地收集了血脂值和主要不良心血管事件。
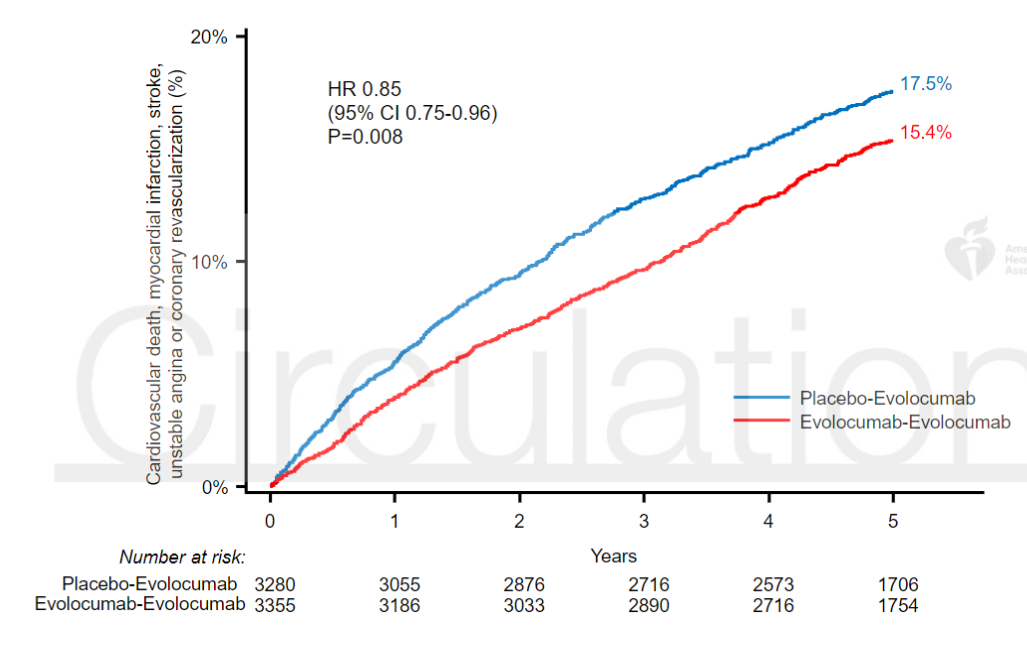
6635例患者入选(3355例随机接受依洛尤单抗,3280例随机接受安慰剂)。中位随访时间为5.0年,依洛尤单抗最长治疗期为8.4年。在第12周时,中位LDL-C为30 mg/dl,依洛尤单抗组63.2%的患者LDL-C<40 mg/dl。依洛尤单抗长期使用的严重不良事件、肌肉相关事件、新发糖尿病、出血性卒中和神经认知事件的发生率没有超过安慰剂治疗的患者,也没有随着时间的推移而增加。在随访期间,随机接受依洛尤单抗相比于安慰剂的患者心血管死亡、心肌梗死、卒中、因不稳定型心绞痛住院或冠状动脉血运重建的风险降低了15%(风险比为0.85 [95%CI为0.75-0.96];P=0.008),心血管死亡、心肌梗塞或卒中的风险降低了20%(风险比为0.80 [0.68-0.93];P=0.003),心血管死亡风险降低了23%(风险比为0.77 [0.60-0.99];P = 0.04)。
由此可见,长期使用依洛尤单抗降低LDL-C与持续较低的不良事件发生率相关。
原始出处:
Michelle L. O'Donoghue,et al.Long-Term Evolocumab in Patients with Established Atherosclerotic Cardiovascular Disease.Circulation.2022.https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.122.061620.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#长期治疗#
68
#粥样硬化性#
61
#粥样硬化#
55
#动脉粥样硬化性心血管疾病#
83
#硬化性#
50
#血管疾病#
75