JACC Heart Fail:AHA 2021丨REVeAL-HF研究:心力衰竭患者风险评估对临床决策和患者预后的影响
2021-11-25 “ 心关注”公众号 “ 心关注”公众号
对HF患者风险的准确评估可以提高临床治疗措施的针对性,从而降低不良事件发生率;然而,相关指南尚未提出如何准确量化HF风险。
研究背景
AHA 2021丨REVeAL-HF
对HF患者风险的准确评估可以提高临床治疗措施的针对性,从而降低不良事件发生率;然而,相关指南尚未提出如何准确量化HF风险。既往众多风险预测工具均来自队列研究或随机对照试验(RCT),但由于计算繁琐、缺乏通用性等原因而未能广泛应用于临床,因此HF患者的风险预测仍有赖于临床医生的主观评估。此前,尚无RCT检验HF风险预测对临床决策和患者预后的影响。因此,本研究通过HF风险模型向临床医生提供住院HF患者1年死亡风险,目的是评估这一风险预测是否有助于临床医生改进治疗决策,从而降低患者的再住院率或死亡率。
研究设计
AHA 2021丨REVeAL-HF

图1 参与REVeAL-HF研究的四个医疗中心分布
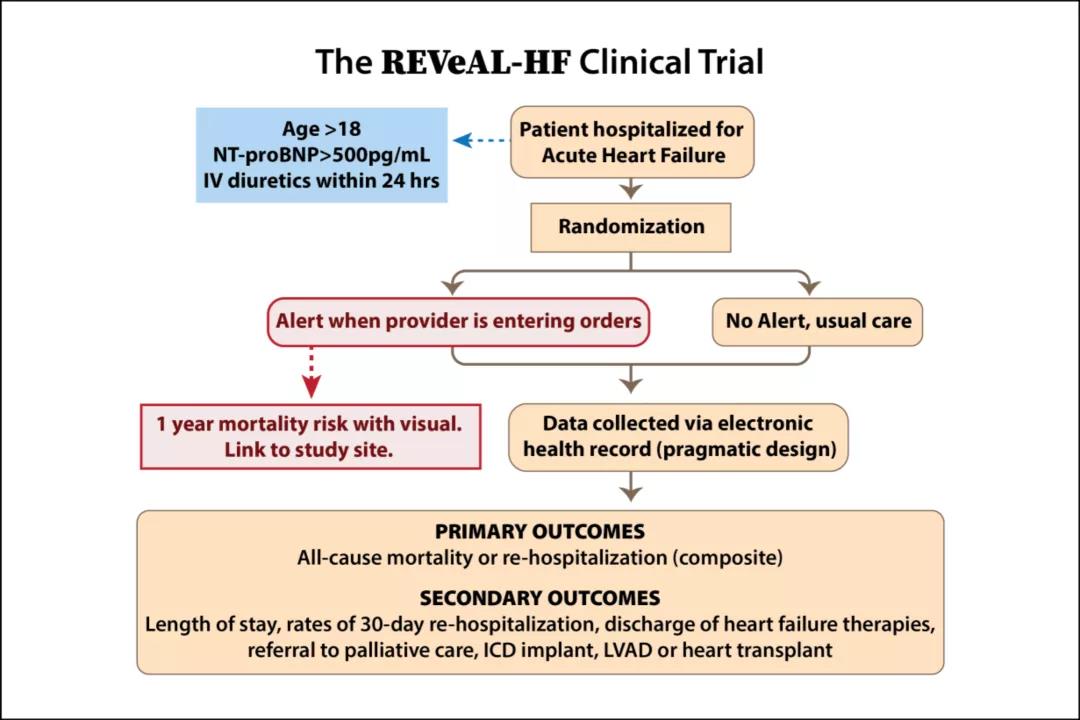
图2 研究设计
本研究是一项多中心RCT,共纳入2019年11月至2021年02月的 3124 名患者,其4个参与中心均为耶鲁纽黑文系统的教学医院(图1)。纳入标准:(1)年龄>18岁;(2)NT-proBNP > 500 pg/ml;(3)24 h内接受静脉利尿剂治疗。
入选患者随机进入干预组和对照组(图2),其中干预组的临床医生会得到来自电子健康档案的数据和耶鲁纽黑文医院(YNHH)HF风险模型提供的住院HF患者1 年预测死亡率(AUC = 0.742,图3、图4)。YNHH HF风险模型纳入因素包括年龄、体重、收缩压、尿素氮、尿素氮/肌酐比值、红细胞平均体积、红细胞分布宽度、单核细胞绝对值、淋巴细胞百分比、肌钙蛋白、NT-proBNP、ICU住院、动脉血 pH 值。评估预知风险对药物、电生理、姑息治疗、心脏移植或机械循环支持等治疗决策和临床结局的影响。

图3 YNHH风险模型预测HF患者1年死亡率的ROC曲线

图4 YNHH HF患者1年死亡率和对应的风险分层
研究主要终点为 30 d内再住院率和死亡率组成的复合终点;次要终点为住院时间、30 d内再住院、HF治疗、转至姑息治疗、转至电生理治疗、植入左心室辅助装置,以及接受心脏移植。
研究结果
AHA 2021丨REVeAL-HF
表1显示了两组患者的基线资料。
表1 两组患者基线情况

终点事件分析:干预组和对照组主要复合终点事件发生率分别为38.9%和39.3%,两组间差异无统计学意义(P = 0.27,图5)。两组患者1年死亡率分别为27.1%和26.9%(P = 0.90);30 d内再住院率分别为19.4%和20.7%(P = 0.39)。亚组分析显示,预知HF风险在年龄≤75岁、肌酐≤ 2.5mg/dL、NTpro-BNP > 1000 pg/ml、危险分层为极低和中风险的干预组人群中为有利因素,但两组间差异均无统计学意义(图6)。
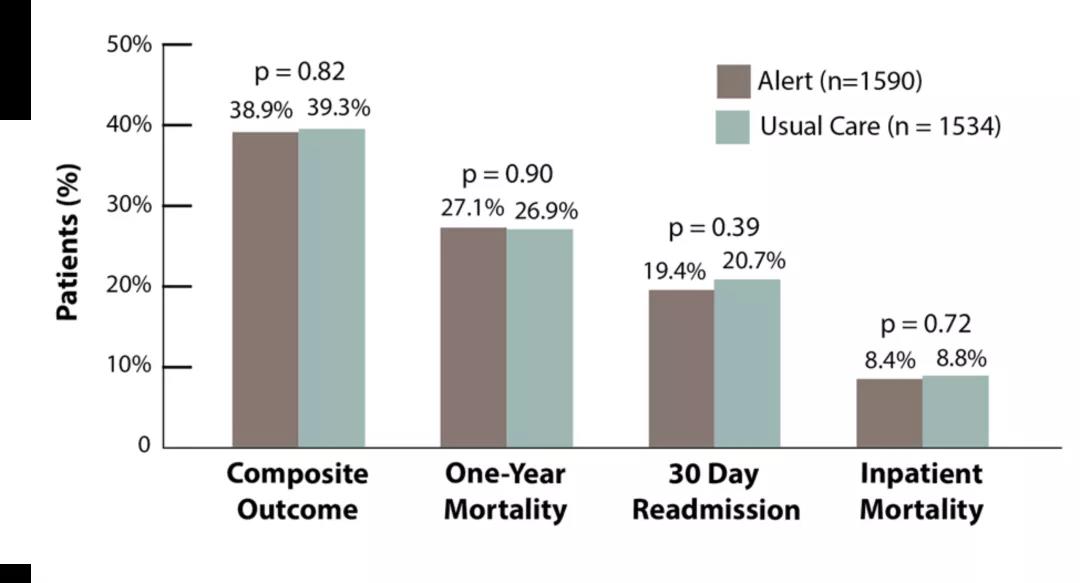
图5 终点事件发生率

图6 亚组分析
在LVEF ≤ 40% 的患者中,两组在β受体阻滞剂(P = 0.32)、血管紧张素转化酶抑制剂/血管紧张素受体拮抗剂/脑啡肽酶抑制剂(ACEI/ARB/ARNI, P = 0.84)、醛固酮受体拮抗剂(MRA, P = 0.47),以及钠-葡萄糖共转运蛋白2(SGLT2)抑制剂(P = 0.29)的使用方面,差异无统计学意义(图7)。不同危险分层下,两组患者姑息治疗的比例差异亦无统计学意义(图7)。在不同危险分层的临床评估中,临床医生对高危组的判断存在差异(P = 0.05),而其余组别的评估差异均无统计学意义(图8)。

图7 两组间药物使用情况和转为姑息治疗的情况分析

图8 不同危险分层临床医生的评估
研究结论
AHA 2021丨REVeAL-HF
向临床医生提供死亡率预测并没有降低HF住院患者的再住院率或死亡率,且死亡率预测对药物治疗、植入型心律转复除颤器(ICD)植入、心脏移植/心室辅助装置,以及或转至姑息治疗等临床决策没有显着影响。未来,临床医生需要更多规范量化的风险评估支持以改进临床决策。
专家点评
AHA 2021丨REVeAL-HF
随着HF发病率的攀升,HF患者的预后也得到了越来越多的关注,准确评估患者风险成为降低HF患者再入院率和死亡率的重要基础。HF治疗策略的制定要基于对患者个体化的风险评估,而准确的评估和临床决策的调整则会在一定程度上影响患者的预后。随着信息化的发展,准确的风险评估模型会发挥越来越大的价值。本研究旨在评估YNHH HF模型所提供的预知风险对临床决策及患者预后的影响,结果显示与常规诊疗相比,利用该模型评估对主要终点事件和临床决策调整的影响均无统计学差异。
目前,HF风险评估主要由临床医生完成,而既往观点认为这种临床评估存在一定主观性。本研究显示,在YNHH HF模型的不同危险等级中,仅高危组临床医生的判断存在偏差,其余组别临床医生的判断与YNHH HF模型是一致的,提示临床医生的判断大多是准确的。
然而,本研究亦存在一定的局限性。首先,YNHH HF模型仅体现出了良好的鉴别效能,但其校准效能较差。其次,YNHH模型能否推广仍待进一步考量;研究仅纳入耶鲁纽黑文健康系统的患者人群,存在一定的时空局限性。此外,该研究受到了 COVID-19的影响,COVID-19导致的额外死亡对其结果会产生一定的影响。
未来,更多准确的HF风险评估模型将得到RCT和大数据的验证并应用于临床,为个体化治疗和精准治疗提供依据,并提高医疗卫生资源的合理应用。
原始出处:
Ahmad Tariq,Yamamoto Yu,Biswas Aditya et al. REVeAL-HF: Design and Rationale of a Pragmatic Randomized Controlled Trial Embedded Within Routine Clinical Practice.[J] .JACC Heart Fail, 2021, 9: 409-419.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#临床决策#
58
#JACC#
26
#患者预后#
32
#AHA#
36
#ACC#
38
#ART#
30
#决策#
40
#HEART#
21
受益匪浅
43