B 细胞活化的可溶性标志物表明 B 细胞在系统性硬化症相关肺动脉高压的发病机制中的作用
2022-08-24 刘少飞 MedSci原创
评估了大型且表型良好的 SSc 人群中几种 B 细胞活化标志物的血清水平,并测试了它们与各种疾病特征(包括器官受累、活动和严重程度)的相关性。
系统性硬化症 (SSc) 是最严重的系统性自身免疫性疾病之一。它的特点是临床三联征,包括免疫异常(自身抗体、高丙种球蛋白血症、急性期反应物升高)、纤维化表现(皮肤、肺和消化道)和血管并发症(如肺动脉高压 (PH)、雷诺现象和手指溃疡)。SSc 是一种异质性疾病,其对患者生活质量的负担是可变的,范围从轻微症状到危及生命的情况。因此,需要开发能够更好地预测和诊断严重器官受累以及准确评估疾病活动和严重程度的工具。
有趣的是,在涉及 B 细胞的其他条件下,一些反映 B 细胞活化的循环蛋白已被证明是有价值的诊断和预后标志物。在系统性红斑狼疮(SLE)患者中,BAFF(B 细胞激活因子)和 APRIL(增殖诱导配体)的血清水平、参与 B 细胞成熟和存活的 2 种细胞因子以及可溶性部分它们的受体 TACI(跨膜激活剂和 CAML 相互作用剂)和 BCMA(B 细胞成熟抗原)升高并与疾病活动相关。APRIL 水平也与狼疮性肾炎的发生有关,并可能预测对免疫抑制剂的反应。在患有各种类型 B 细胞淋巴瘤的患者中,可溶性 CD23 (sCD23)、sCD27 和 sCD30 的血清浓度在诊断前几年就会升高。CXCL13(CXC 基序趋化因子 13)(一种已知可吸引 B 细胞的趋化因子)的循环水平升高,与 SLE、干燥综合征、类风湿性关节炎和 ANCA 相关性血管炎患者的疾病活动、严重程度和治疗反应相关。然而,在 SSc 领域,此类标记的相关性尚未得到广泛研究;这主要是在样本量小的古代研究中完成的。
为了解决这个问题,我们评估了大型且表型良好的 SSc 人群中几种 B 细胞活化标志物的血清水平,并测试了它们与各种疾病特征(包括器官受累、活动和严重程度)的相关性。我们发现 B 细胞生物标志物与肺动脉高压 (PAH) 之间存在关联;并证明 B 细胞可以在 SSc 患者中产生血管生成介质。
研究方法:
1. 14种B细胞生物标志物(β2-微球蛋白、类风湿因子(RF)、免疫球蛋白(Ig)G、IgA、IgM、BAFF、APRIL、可溶性(s)TACI、sBCMA、sCD21、sCD23、sCD25、sCD27)的血清水平, CXCL13) 在 SSc 患者和健康对照 (HC) 中测量。2. 评估了这些生物标志物与 SSc 特征之间的关联。3. 通过研究 B 细胞培养上清液中的蛋白质产生,探索了已确定关联的病理生理学相关性。
研究结果:
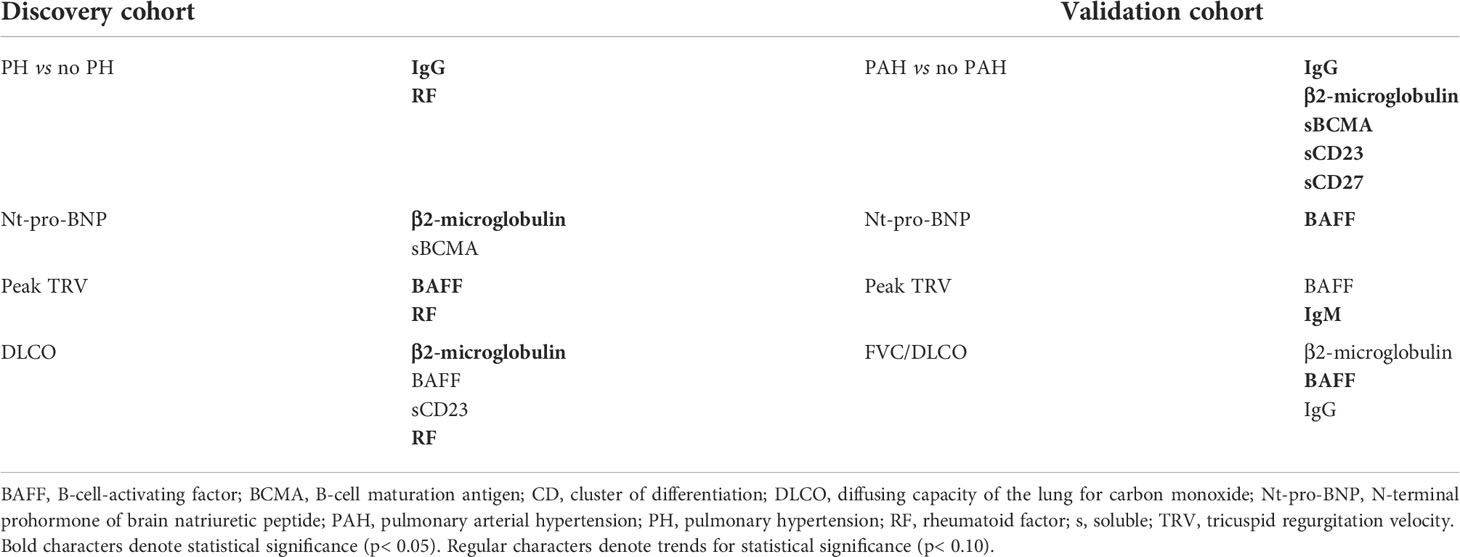
在包含广泛疾病表现的 80 名 SSc 患者的发现小组中,我们观察到与 HC 相比,RF 阳性频率更高,β2-微球蛋白、IgG 和 CXCL13 水平升高。我们发现几种生物标志物与与疾病表型、活动和严重程度相关的 SSc 特征之间存在显着关联。尤其是血清 IgG 水平与肺动脉高压(PH)相关;具有 Nt-pro-BNP 和 DLCO 的 β2-微球蛋白;和具有峰值三尖瓣反流速度 (TRV) 的 BAFF。在没有广泛 ILD 的有限皮肤 SSc 患者的验证队列中,我们观察到肺动脉高压 (PAH) 患者的血清 IgG 水平较低,而 β2-微球蛋白、sBCMA、sCD23 和 sCD27 水平较高。BAFF 水平与 Nt-pro-BNP 水平密切相关,SSc-PAH 患者的 FVC/DLCO 比值和峰值 TRV。与 HC 相比,培养的 SSc B 细胞显示出各种血管生成因子(血管生成素、血管生成素-1、VEGFR-1、PDGF-AA、MMP-8、TIMP-1、L-选择素)的生成增加,血管生成素-2 的生成减少。
研究结论:
B 细胞活化的可溶性标志物可能是评估 SSc 器官受累、活动和严重程度的相关工具。它们与 PAH 的关联可以证明 B 细胞活化在肺微血管病发病机制中的作用。B 细胞可能通过产生血管生成介质导致 SSc 血管病变。
参考文献:
Sanges S, Guerrier T, Duhamel A, Guilbert L, Hauspie C, Largy A, Balden M, Podevin C, Lefèvre G, Jendoubi M, Speca S, Hachulla É, Sobanski V, Dubucquoi S, Launay D. Soluble markers of B cell activation suggest a role of B cells in the pathogenesis of systemic sclerosis-associated pulmonary arterial hypertension. Front Immunol. 2022 Jul 29;13:954007. doi: 10.3389/fimmu.2022.954007. PMID: 35967377; PMCID: PMC9374103.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#动脉高压#
0
#硬化症#
69
#标志物#
39
#系统性#
39
😊😊😊
51
#系统性硬化#
48