Cell:哈佛大学重磅糖尿病“突破”正式宣布撤稿!
2017-01-01 生物探索 生物探索
导读:本周,一篇2013年发表在Cell杂志上的糖尿病突破成果正式宣布撤稿。这篇论文发表时引起了强烈的关注,因为它提出了利用机体自身机制调控胰岛素产生的方法,为糖尿病患者摆脱注射治疗带来了希望。Harvard stem cell scientist Doug Melton, standing, in his lab with post-doc Peng Yi, the lead author of
导读:本周,一篇2013年发表在Cell杂志上的糖尿病突破成果正式宣布撤稿。这篇论文发表时引起了强烈的关注,因为它提出了利用机体自身机制调控胰岛素产生的方法,为糖尿病患者摆脱注射治疗带来了希望。

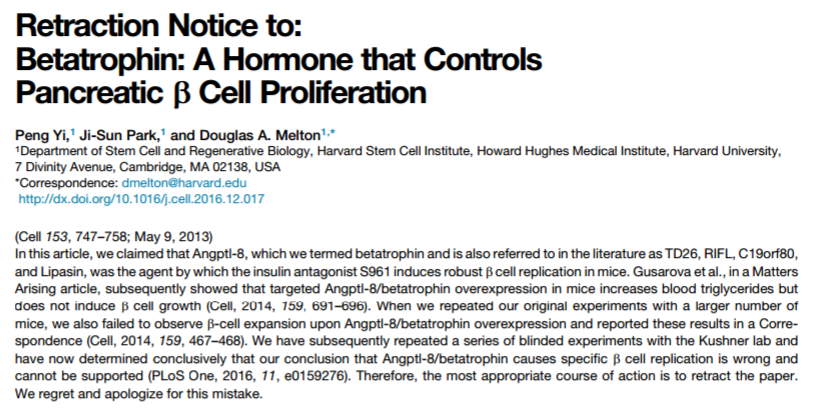
2016年12月27日,Cell杂志发布了一条撤稿通知(下图),宣布2013年发表在该杂志上题为“Betatrophin: A Hormone that Controls Pancreatic β Cell Proliferation”的论文正式撤稿。在这篇文章,来自哈佛大学的科学家小组在肝脏中发现的一种名为betatrophin的激素能够在小鼠中控制胰岛β细胞增殖。
这篇论文发表时引起了强烈的关注,因为它提出了利用机体自身机制调控胰岛素产生的方法,为糖尿病患者摆脱注射治疗带来了希望。
参与这项研究的3位作者在撤稿通知中指出,2014年10月,发表在Cell杂志上发表的题为“ANGPTL8/Betatrophin Does Not Control Pancreatic Beta Cell Expansion”的文章指出,小鼠肝脏中betatrophin过表达增加了血浆中的甘油三酯水平,但并没有诱导β细胞的生长。Regeneron制药的Viktoria Gusarova是该研究的通讯作者兼第一作者。
当哈佛大学的研究小组在更多数量的小鼠中重复他们的实验时,也没有观察到基于betatrophin过表达的β细胞增殖。在Gusarova等人发表上述相反结果的同时,哈佛大学的研究小组也于同日在Cell杂志发表了题为“Perspectives on the Activities of ANGPTL8/Betatrophin”的Correspondence文章。
之后,研究小组与贝勒医学院Jake A. Kushner 的实验室合作,重复了多次实验,最终证明,betatrophin导致β细胞复制的结论是错误的。相关结果于今年7月发表在PLoS One杂志上(题目:Resolving Discrepant Findings on ANGPTL8 in β-Cell Proliferation: A Collaborative Approach to Resolving the Betatrophin Controversy)。
哈佛大学的研究人员在撤稿通知表示,他们对这一错误深表遗憾和歉意。原研究的通讯作者Douglas A. Melton说:“就像任何撤稿一样,这是令人失望的。但是对betatrophin假说的否定过程说明了当科学家意见不一致时是如何共同努力,推动领域的发展。”
Melton是干细胞研究领域的先驱者之一。上世纪90年代初,他的儿子被诊断为1型糖尿病。他一直致力于将干细胞转化为β细胞,希望能够用于治愈糖尿病。我们祝愿在2017年,科学家们能够取得新的研究进展,帮助数亿糖尿病患者。
原始出处:
[1] Peng Yi,et al. Retraction Notice to: Betatrophin: A Hormone that Controls Pancreatic β Cell Proliferation. Cell.2016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
29
#CEL#
23
每天学习一点
50
有意思咯,啥原因呢?
54
#重磅#
30
#哈佛#
32