JAMA Oncol:纳武利尤单抗(Nivolumab)联合伊匹木单抗(Ipilimumab)对比纳武利尤单抗治疗既往治疗过的IV期鳞状非小细胞肺癌的疗效:3期临床研究Lung-MAPS1400I
2021-07-17 yd2015 MedSci原创
该3期临床研究表明,在既往治疗过的,但是没有使用过免疫治疗的IV期鳞状NSCLC患者中,在nivolumab的基础上加上ipilimumab并不能改善患者的预后。
晚期非小细胞肺癌中,纳武利尤单抗(Nivolumab)联合伊匹木单抗(Ipilimumab)一线治疗较铂类为基础的化疗改善患者的预后。晚期NSCLC患者二线治疗中,Nivolumab也较多西他赛改善患者的预后。那么,在既往治疗过的但是没有使用过免疫治疗的IV期鳞状非小细胞肺癌中,在纳武利尤单抗(Nivolumab)基础上加上伊匹木单抗(Ipilimumab)能否改善患者的预后呢?因此,有研究者开展了3期临床研究Lung-MAPS1400I,旨在评估纳武利尤单抗(Nivolumab)联合伊匹木单抗(Ipilimumab)对比纳武利尤单抗治疗既往治疗过的IV期鳞状非小细胞肺癌的疗效和安全性。相关成果发表在JAMA Oncology杂志上。
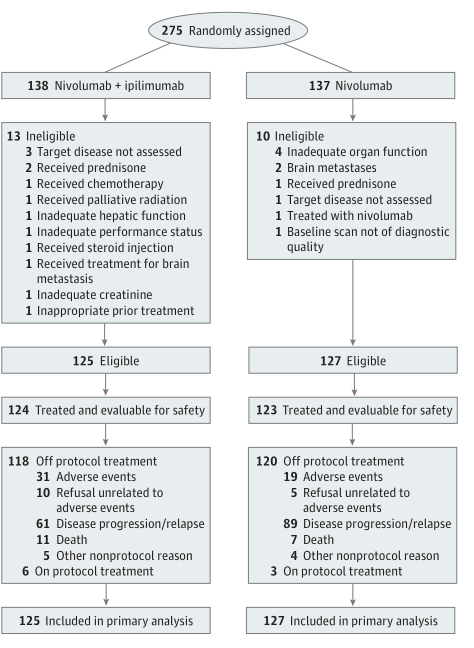
Lung-MAPS1400I研究是3期开放标签随机试验。患者被随机1:1分配至Nivolumab联合Ipilimumab组或Nivolumab组。Nivolumab 治疗量为3mg/kg/2周,Ipilimumab为1mg/kg/6周,直至疾病进展或不可耐受毒性。主要研究终点为OS,次要终点为研究者评估的PFS(IA-PFS)和ORR。
研究概况
纳入275例患者,其中252例患者可评估,Nivolumab联合Ipilimumab组为125例,Nivolumab组为127例。Nivolumab联合Ipilimumab组和Nivolumab组的中位OS分别为10个月(95%CI,8.0-14.4)和11个月(95%CI,8.6-13.7),没有统计学差异(HR=0.87;95% CI,0.66-1.16;P =0 .34)。两组的1年和2年OS率分别为45%(95%CI,37%-55%) vs 44%(95% CI, 36%-54%) 和28%(95%CI,21%-37%) vs 22% (95% CI, 15%-30%)。
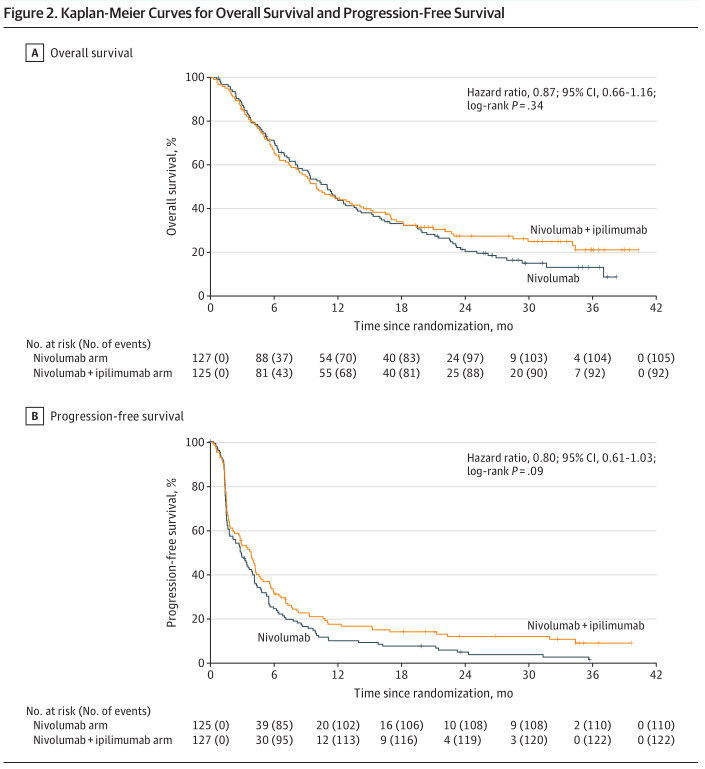
OS 和PFS
两组的中位IA-PFS分别为3.8个月(95%CI,2.7-4.4)和2.9个月(95%CI,1.8-4.0),同样也没有明显统计学差异 (HR=0.80, 95%CI,0.61-1.03;P =0.09)。两组的1年和2年PFS率分别为17% (95% CI, 12%-25%) vs 10% (95% CI, 6%-17%) 和12% (95% CI, 7%-19%) vs 5%(95%CI,2%-10%)。
两组的ORR分别为18% (95%CI,12%-25%)和17%(95%CI,10%-23%)。中位缓解持续时间分别为28.4个月(95%CI,4.9-未达到)和9.7个月(95%CI,4.2-23.1)。
在TMB≥10 mt/Mb和PD-L1 < 1%患者中,nivolumab 联合 ipilimumab较nivolumab治疗改善患者的预后(HR=0.37;95% CI, 0.15-0.89; P = 0.02);而在TMB<10 mt/Mb和PD-L1 < 1%患者中,nivolumab 联合 ipilimumab反而导致更差的预后(HR=2.46; 95% CI, 0.95-6.34; P = 0.06)。在PD-L1≥1%患者中,无论TMB水平,两组的预后都没有统计学差异。
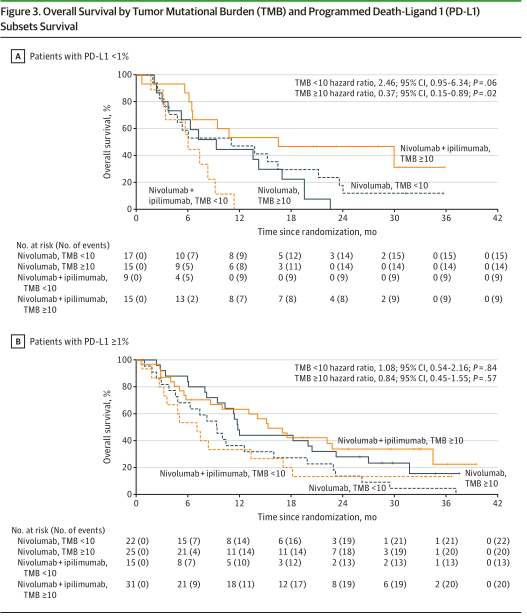
PD-L1和TMB分层的OS比较
两组≥3级治疗相关不良事件的发生率分别为39.5%和33.3%;毒性导致治疗中断的比例分别为25%和15%。常见的有包括疲劳(8.9%和5.7%)和肺炎(7.3%和4.9%)。治疗相关性死亡发生在nivolumab 联合 ipilimumab组有2.4%,而nivolumab组有0.8%。
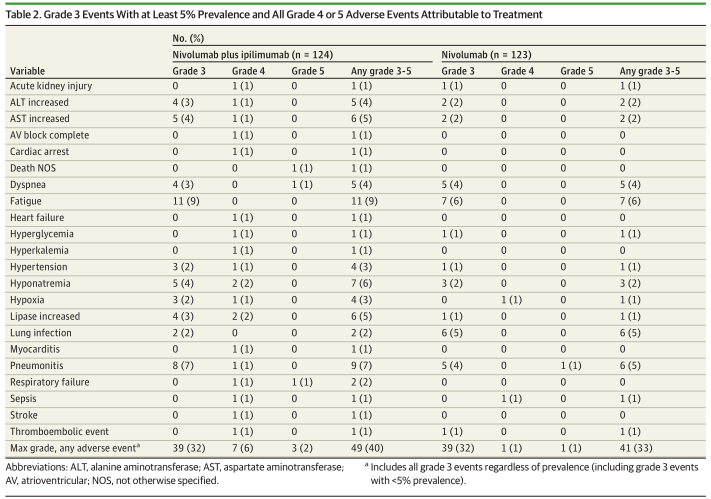
不良反应
综上,该3期临床研究表明,在既往治疗过的,但是没有使用过免疫治疗的IV期鳞状NSCLC患者中,在nivolumab的基础上加上ipilimumab并不能改善患者的预后。
原始出处:
ScottN.Gettinger; MaryW.Redman; LyudmilaBazhenova, et al. Nivolumab Plus Ipilimumab vs Nivolumab for Previously Treated Patients With Stage IV Squamous Cell Lung Cancer: The Lung-MAPS1400I Phase 3 Randomized Clinical Trial. JAMA Oncol. doi:10.1001/jamaoncol.2021.2209. PublishedonlineJuly15,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#3期临床#
78
#mAb#
0
#伊匹木单抗#
60
#Oncol#
45
#非小细胞#
47
#Ipilimumab#
51
#APS#
61
收藏TMB>10的,待研究
77
#NIV#
39
学习
0