Lancet:乌司奴单抗治疗活动性SLE的疗效和安全性:一项多中心、双盲、2期、随机、对照研究结果
2018-10-17 MedSci MedSci原创
van Vollenhoven RF等研究者于2018年9月21日在Lancet上在线发表了一篇研究,旨在评价乌司奴单抗治疗经常规治疗无效的中度至重度疾病活动性系统性红斑狼疮(SLE)患者的疗效和安全性。 乌司奴单抗是一种靶向白介素-12(IL-12)和白介素-23(IL-23)的单克隆抗体,已被批准用于斑块型银屑病、银屑病关节炎及克罗恩病的治疗。既往研究显示,IL-12和IL-23与SLE
van Vollenhoven RF等研究者于2018年9月21日在Lancet上在线发表了一篇研究,旨在评价乌司奴单抗治疗经常规治疗无效的中度至重度疾病活动性系统性红斑狼疮(SLE)患者的疗效和安全性。
乌司奴单抗是一种靶向白介素-12(IL-12)和白介素-23(IL-23)的单克隆抗体,已被批准用于斑块型银屑病、银屑病关节炎及克罗恩病的治疗。既往研究显示,IL-12和IL-23与SLE有关。
这是一项在阿根廷、澳大利亚、德国、匈牙利、墨西哥、波兰、西班牙、台湾和美国44家私人诊所和学术中心针对活动性血清学阳性SLE成年患者开展的多中心、双盲、2期、随机、对照试验。纳入的成年患者年龄为18~75岁,体重至少35kg,在首次服用研究药物前至少3个月诊断为SLE。符合纳入标准的患者被随机分配(按照3:2的比例)至乌司奴单抗组或安慰剂组,并根据皮肤活检、存在狼疮性肾炎、基线SLE药物和SLE疾病活动指数2000(SLEDAI-2K)评分综合因素、地点、区域和种族进行分层。患者和研究人员均不知晓治疗药物分配。两组除进行标准治疗之外,患者接受静脉注射乌司奴单抗(体重35~55kg的患者给药剂量为260mg,体重>55kg且≤85kg的患者给药剂量为390mg,体重>85kg的患者给药剂量为520mg),随后每8周一次皮下注射乌司奴单抗90mg,或在第0周静脉注射安慰剂,随后每8周一次皮下注射安慰剂。主要终点是在第24周达到SLIDAI-2K应答者指数-4(SRI-4)应答的患者百分比。对接受至少一次随机分配的研究药物给药(部分或完全、静脉注射或皮下注射)的改良意向性治疗人群进行疗效分析。对所有接受至少一次研究药物治疗的患者进行安全性分析,而不考虑分配组。
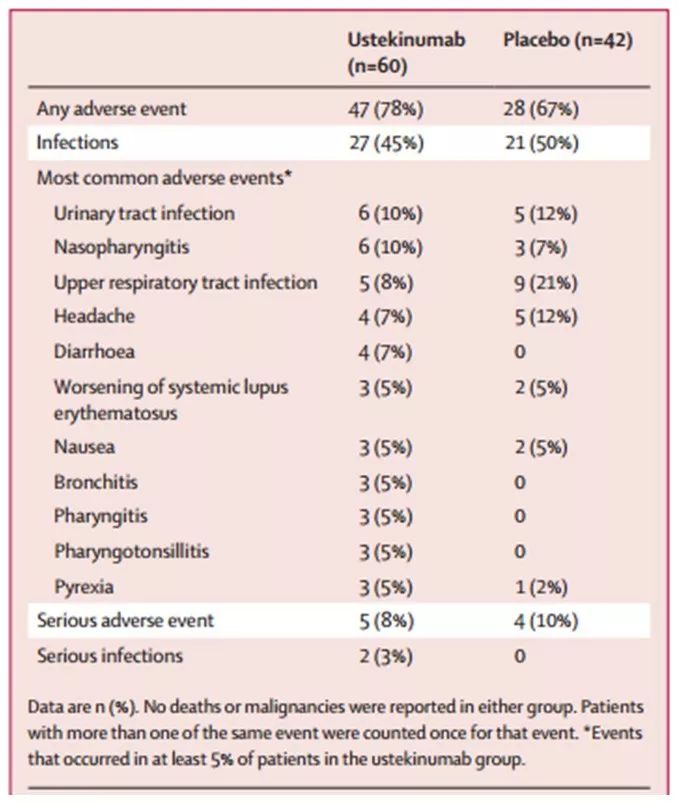
该研究结果显示,从2015年10月6日至2016年11月30日,筛选了166例患者,其中102例被随机分配至接受乌司奴单抗(n=60)或安慰剂(n=42)治疗。在第24周,乌司奴单抗组60例患者中有37例(62%)获得SRI-4应答,安慰剂组42例患者中有14例(33%)获得SRI-4应答(百分比差异为28%,95%CI:10~47,P=0.006)(表1 & 图1 A)。接受乌司奴单抗的患者在12周至24周期间发生大不列颠群岛狼疮评估组指数(BILAG)复发的可能性显著低于接受安慰剂的患者[危险比(HR):0.12,95%CI:0.01~1.04,P=0.012](图1B)。在24周内,乌司奴单抗组47例(78%)患者和安慰剂组28例(67%)患者发生至少1次不良事件(表2)。感染是最常见的不良事件类型[乌司奴单抗组27例(45%),安慰剂组21例(50%)]。0~24周内未发生死亡或治疗后引起的机会性感染、带状疱疹、结核病或恶性肿瘤。
表1. 24周疗效
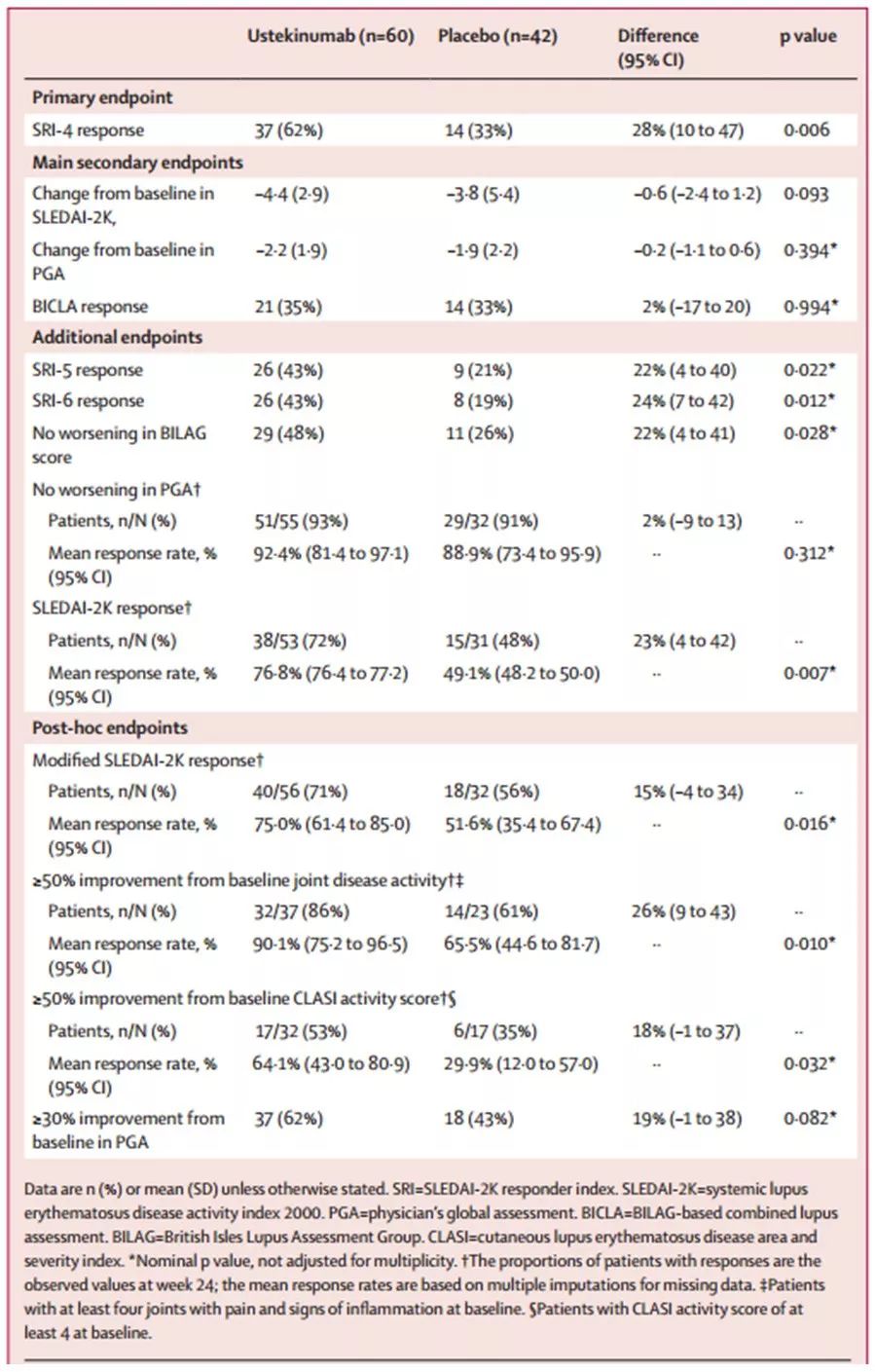
图1. 0~24周SRI-4 应答(图A)以及12~24周至BILAG复发的时间(图B)
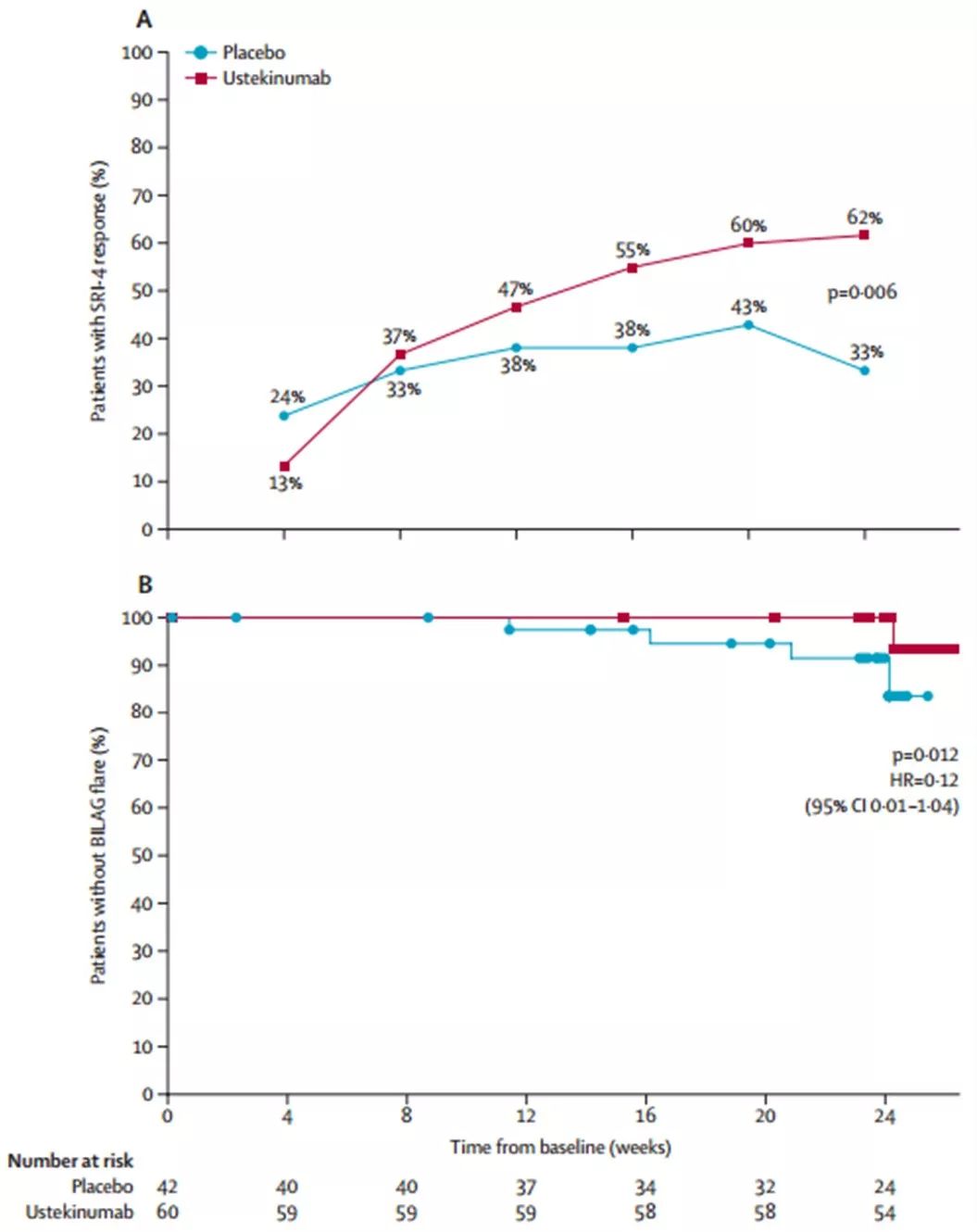
表2. 24周内发生不良事件的患者数
总之,标准治疗加用乌司奴单抗相比安慰剂治疗活动性SLE,可获得更好的临床和实验室指标方面的疗效,而其安全性与乌司奴单抗治疗其他疾病的结果一致。该研究结果支持进一步探讨乌司奴单抗作为SLE的新疗法。
内容要点:
-
该研究之前的证据
研究者们在2018年5月29日检索了PubMed,查找截止至2018年5月29日的英语报告,检索术语包括“ustekinumab”、“lupus”、“systemic lupus erythematosus”、“SLE”、“anti-interleukin-12”、“anti-interleukin-23”以及“anti-interleukin-17”。未发现乌司奴单抗或其他抗IL-12/23p40药物、抗IL-23p19或抗IL-17或抗IL-17受体药物治疗SLE患者疗效方面的研究。文献报道IL-12和IL-23通路参与SLE发病机制。乌司奴单抗是一种单克隆抗IL-12和IL-23抗体,被批准用于成人银屑病关节炎和克罗恩病以及成人和青少年斑块型银屑病患者。 -
该研究的附加价值
据研究者所知,这是首项乌司奴单抗治疗活动性SLE患者的2期、随机、安慰剂对照研究。24周时,接受乌司奴单抗治疗患者的临床参数(总体SLE疾病活动反应指数、关节计数、皮肤粘膜疾病以及疾病复发)和实验室参数(C3补体浓度和抗dsDNA自身抗体)相比安慰剂治疗患者有更多改善。安全性结果与已知的乌司奴单抗安全性一致。这些结果有力地支持开展进一步研究探讨乌司奴单抗治疗SLE患者的新作用机制。 -
所有现有证据的意义
B细胞靶向治疗SLE的研究成果不一,标准治疗具有相当大的毒性,近六十年来仅有一种具有新作用机制的药物被批准用于SLE。因此,针对这些患者仍存在显著未被满足的需要。该研究结果表明乌司奴单抗可能是治疗SLE的有效方法。乌司奴单抗治疗SLE患者的疗效和安全性正在3期试验中进一步评估。
参考文献:
van Vollenhoven RF, Hahn BH, Tsokos GC, et al. Efficacy and safety of ustekinumab, an IL-12 and IL-23 inhibitor, in patients with active systemic lupus erythematosus: results of a multicentre, double-blind, phase 2, randomised, controlled study.Lancet. 2018 Sep 21.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#研究结果#
31
#疗效和安全性#
36
#对照#
47
#活动性#
40
#多中心#
46
#Lancet#
24
#SLE#
31
#双盲#
25
谢谢梅斯提供这么好的信息,学到很多
47