干细胞疗法治疗重症COVID-19患者:双盲安慰剂对照试验已证明JadiCells的有效性
2021-01-07 Allan MedSci原创
制药公司Creative Medical Technology Holdings近日宣布,
制药公司Creative Medical Technology Holdings近日宣布,静脉内给药脐带衍生干细胞(JadiCells)可显著提高重症COVID-19患者的存活率。
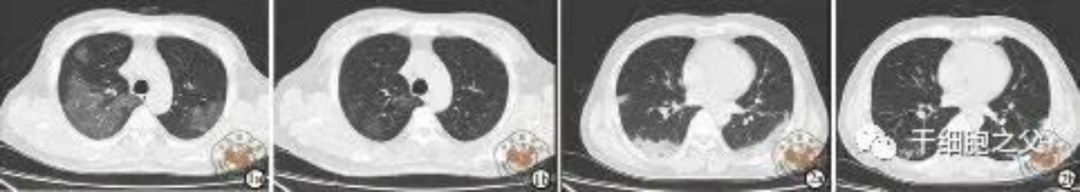
I/II期双盲、安慰剂对照试验在第0天和第3天用1亿个JadiCells静脉注射治疗了12例重症COVID-19患者,另有12例患者接受了安慰剂治疗。在28天时,接受JadiCells治疗的患者中有91%存活,而安慰剂组中只有42%的患者存活。在JadiCells组中未见任何不良反应。

Creative Medical Technology Holdings总裁兼首席执行官Timothy Warbington说道:“今天报道的数据强烈支持JadiCells的安全性和有效性”。
间充质干细胞是一种强大的免疫调节剂,这种细胞分泌许多抗炎生物活性物质(细胞因子),从而减少肺部的炎症过程。而且,间充质干细胞分泌很多生长因子,这些因子不仅有助于受损伤的肺组织恢复,而且还有助于其他器官的恢复。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#DIC#
37
#对照#
37
#CEL#
40
#对照试验#
31
学习
80
好文章,分享
0
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
62
#干细胞疗法#
48
#COVID-19患者#
36
#双盲#
31