JAMA子刊:严重肥胖患者全髋关节置换术并发症风险评估
2021-09-05 MedSci原创 MedSci原创
骨关节炎是全世界疼痛、残疾和卫生保健资源使用的主要原因之一。
骨关节炎是全世界疼痛、残疾和卫生保健资源使用的主要原因之一。虽然这种疾病可以影响任何关节,但髋关节是最常见的受累部位。由于人口老龄化,骨关节炎的发病率也越来越高,因此,个人和社会层面的经济负担将继续增加。
髋关节置换手术是严重髋关节骨关节炎患者的不二之选。据统计,从2018年到2030年,初次全髋关节置换的使用预计将增加71%。在美国,典型的髋关节置换手术花费从17763到239696美元不等,并且每年累计花费美国医疗保健系统150亿美元。值得注意的是,该支出仅代表与该手术相关的费用的一部分,随后的康复估计每年花费超过1.804亿美元。
肥胖是包括全髋关节置换术(THA)在内的许多外科手术后主要并发症的风险因素。3级或严重肥胖(BMI≥40)尤其与THA后手术部位感染、脱位、假体早期松动、翻修手术、假体周围骨折和血栓栓塞的风险增加有关。同时,肥胖症患者对TJA的需求持续增加。
尽管有较高的并发症风险,但肥胖患者在THA后的功能和生活质量也有类似的改善。为了确定外科医生对严重肥胖患者的THA经验与并发症风险之间的关系,来自加拿大桑尼布鲁克健康科学中心的专家开展了相关研究,结果发表在JAMA Network Open杂志上。
这项基于人群的回顾性队列研究在加拿大安大略省进行,时间为2007年4月1日至2017年3月31日。定义了一个因骨关节炎而接受初级THA的患者队列,这些患者在手术时有严重的肥胖症(BMI≥40)。在控制了潜在的混杂因素后,使用广义估计方程来确定总体THA和严重肥胖特定THA外科医生数量与并发症发生之间的关系。
主要暴露因素是进行THA。并发症被认为是手术后1年内的综合结果(翻修、需要手术的感染或需要复位的脱位)。结果共有4781名符合条件的患者纳入。中位年龄为63岁(四分位数范围[IQR],56-69),3050名患者(63.8%)为女性。
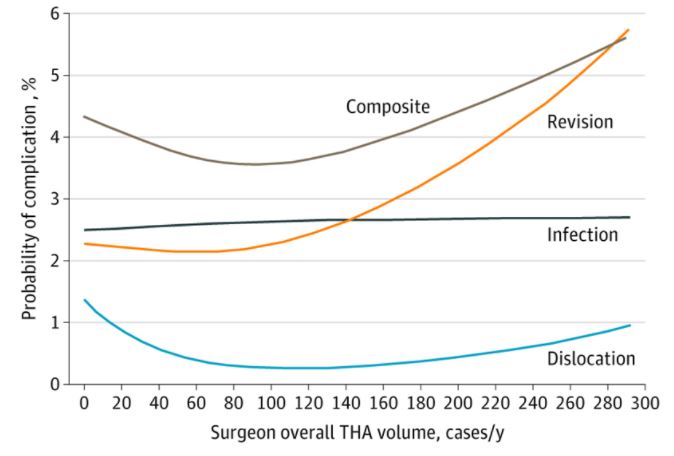
按外科医生的全髋关节置换术总量计算,严重肥胖患者在THA后出现并发症的概率
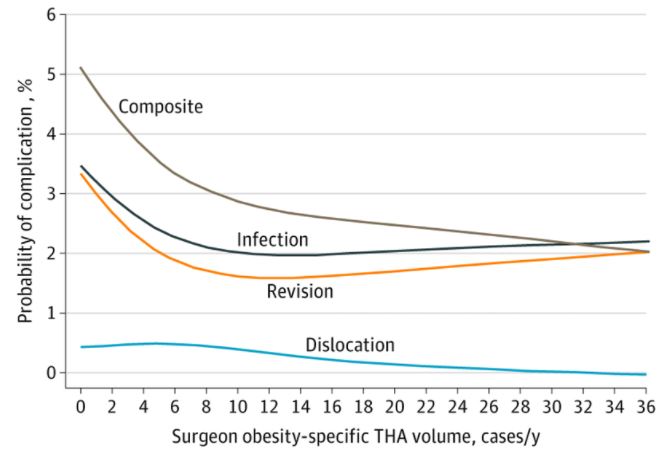
总体而言,186名患者(3.9%)在手术后一年内出现了手术并发症。整体THA外科医生的手术量中位数为70(IQR,46-106)例/年,而肥胖症特定外科医生的手术量中位数为5(IQR,2-9)例/年。在控制了病人和医院的因素后,更多的肥胖特异性THA外科医生的手术量(每增加10例调整后的几率比为0.65,95% CI:0.47-0.89)能降低35%并发症的风险,而整体THA外科医生的手术量(每增加10例调整后的几率比为0.97;95% CI:0.93-1.02)则无关。
按外科医生特定肥胖的THA量计算,重肥胖患者在THA后出现并发症的概率
综上,外科医生对严重肥胖患者进行THA的经验增加与较少的主要手术并发症有关。这些发现表明,外科医生需要有经验来减轻严重肥胖患者手术带来的独特的解剖学挑战。应该考虑将严重肥胖症患者转诊到具有高肥胖症特定THA手术量的外科医生处。
参考文献:
Association of Surgical Experience With Risk of Complication in Total Hip Arthroplasty Among Patients With Severe Obesity. JAMA Netw Open. 2021;4(9):e2123478. doi:10.1001/jamanetworkopen.2021.23478
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




















#置换#
39
#全髋关节#
56
#并发#
30
#关节置换术#
75
#肥胖患者#
44
感谢分享
54
#置换术#
31
学习了,谢谢分享
64
学习
56
显而易见的结论用理论来表示
63