Clin Cancer Res:陈明教授团队发现不可手术的食管鳞状细胞癌(ESCC)同步放化疗中使用放疗剂量为50Gy更合适
2022-03-11 yd2015 MedSci原创
研究表明,60Gy和50Gy同步放化疗治疗不可手术ESCC患者疗效相当,但60Gy组严重肺炎发生率高,因此,50Gy可能是更好的推荐剂量。
不可手术的食管鳞状细胞癌(ESCC)患者常应用同步放化疗(CCRT)治疗,而最佳的放疗剂量尚不明确。因此,来自浙江省肿瘤医院的陈明教授团队开展了一项多中心III期临床研究,主要是评估同步放化疗中60Gy对比50Gy剂量的疗效和安全性。相关结果发表在Clin Cancer Res杂志上。
研究纳入病理证实为IIA期-IVA期ESCC患者,随机1:1分配至接受60Gy或50Gy常规分割(肿瘤和区域淋巴结)的放疗。同步给予每周化疗(多西他赛25 mg/m2;顺铂25 mg/m2)和2个周期的巩固化疗(多西他赛70 mg/m2;顺铂25mg /m2, d1 ~ 3)。
2013年5月10日至2017年5月16日,22个中心共有324名患者被随机分配接受60 Gy(实验组,n = 161)或50 Gy(对照组(n = 163)治疗。5例患者随访缺失;因此,319例患者被定义为全分析集人群纳入分析。
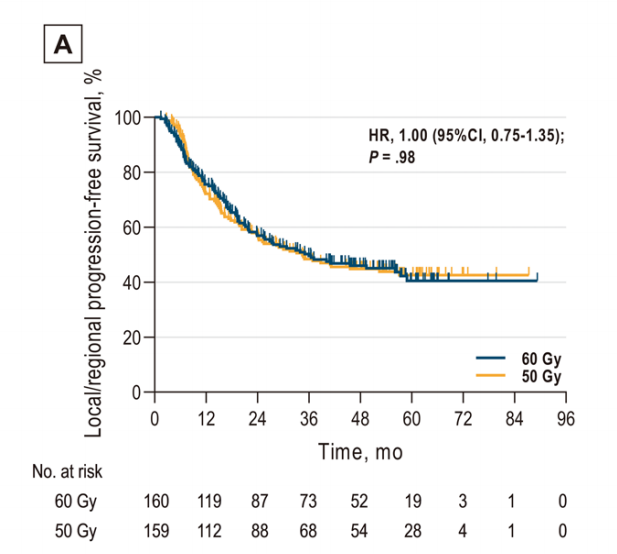
319例患者的中位随访时间为34.0个月,153例仍存活患者的中位随访时间为55.2(1.5-89.3)个月。两组的LRPFS, OS,或 PFS率没有统计学差异。60Gy和50Gy两组的1年、2年和3年LRPFS率分别为75.6%、56.9%、49.5% 和72.1%、57.2%和48.4%;而中位LRPFS分别为36.0和34.5个月(HR, 1.00;95%CI,0.75 - 1.35;P = 0.98)。
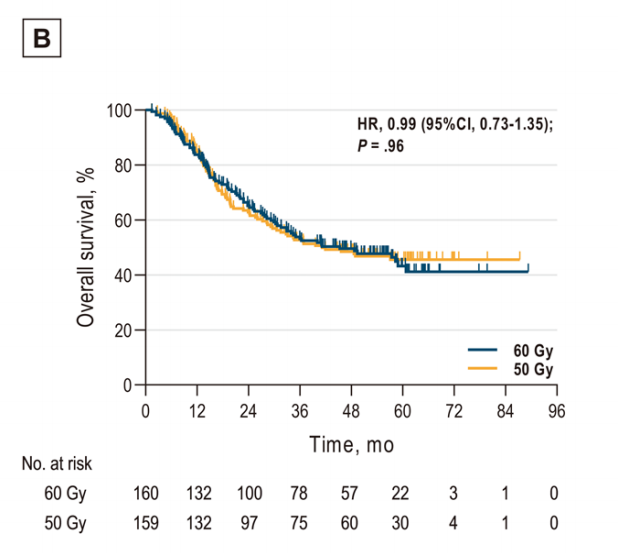
两组的1年、2年和3年OS率分别为83.7%、65.1、53.1%和84.8%, 62.8%, and 52.7%,中位OS分别为45.3个月和41.2个月(HR, 0.99;95%CI,0.73 - 1.35;P = 0.96)。
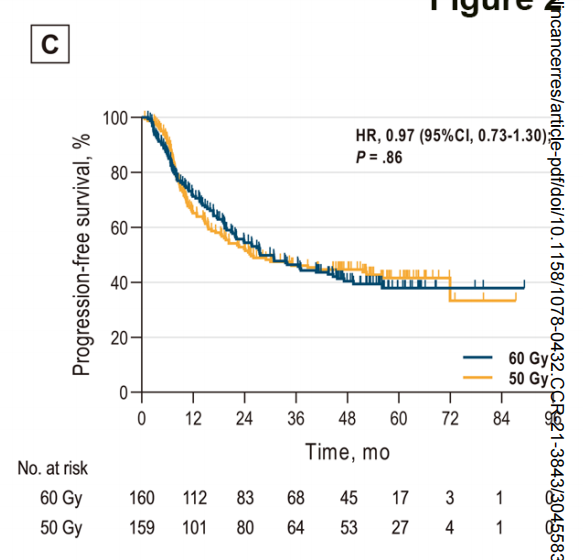
两组的1年、2年和3年PFS率分别为71.2%、54.4%、46.4%和65.2%、52.1%、46.1% ,中位PFS分别为27.7和25.5个月(HR, 0.97;95%CI,0.73 - 1.30;P = 0.86)。
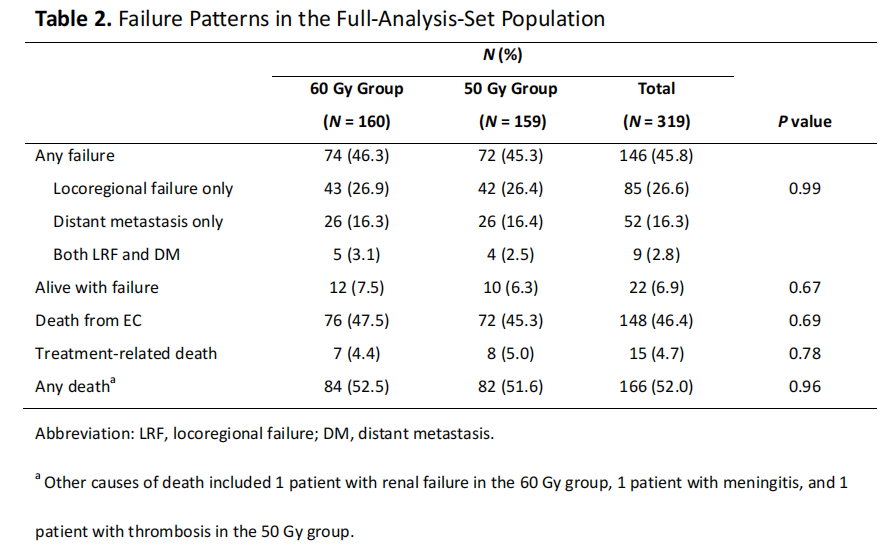
60Gy和50Gy组的任何进展率分别为46.3%和45.3%,包括局部区域进展率为26.9%和26.4%,远处转移为16.3%和16.4%,以及同时局部区域和远处转移率分别为3.1%和2.5%;这些值无显著差异。
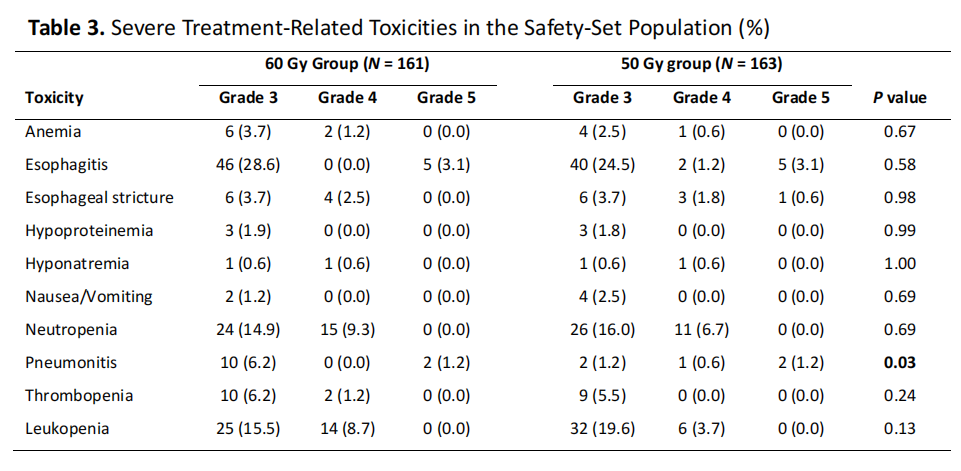
60Gy组中54.7%的患者发生了3级或3级以上的不良事件,50Gy组为50.9% (P = 0.50)。60 Gy组3级或以上放射相关肺炎的发生率高于50 Gy组(7.5% vs 3.1%,P = 0.03)。
综上,研究表明,60Gy和50Gy同步放化疗治疗不可手术ESCC患者疗效相当,但60Gy组严重肺炎发生率高,因此,50Gy可能是更好的推荐剂量。
原始出处:
Xu Y, Dong B, Zhu W, Li J, Huang R, Sun Z, Yang X, Liu L, He H, Liao Z, Guan N, Kong Y, Wang W, Chen J, He H, Qiu G, Zeng M, Pu J, Hu W, Bao Y, Liu Z, Ma J, Jiang H, Du X, Hu J, Zhuang T, Cai J, Huang J, Tao H, Liu Y, Liang X, Zhou J, Tao G, Zheng X, Chen M. A phase III multicenter randomized clinical trial of 60 Gy vs 50 Gy radiation dose in concurrent chemoradiotherapy for inoperable esophageal squamous cell carcinoma. Clin Cancer Res. 2022 Feb 18:clincanres.3843.2021. doi: 10.1158/1078-0432.CCR-21-3843. Epub ahead of print. PMID: 35190815.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#SCC#
51
#细胞癌#
32
#放化疗#
67
#食管鳞状细胞癌#
66
#食管#
39
#同步放化疗#
47
#ESCC#
49
好文章,值得一读。
50