中枢性完全性尿崩症1例
2017-12-28 王绵 张力辉 殷立新 内分泌系统疾病
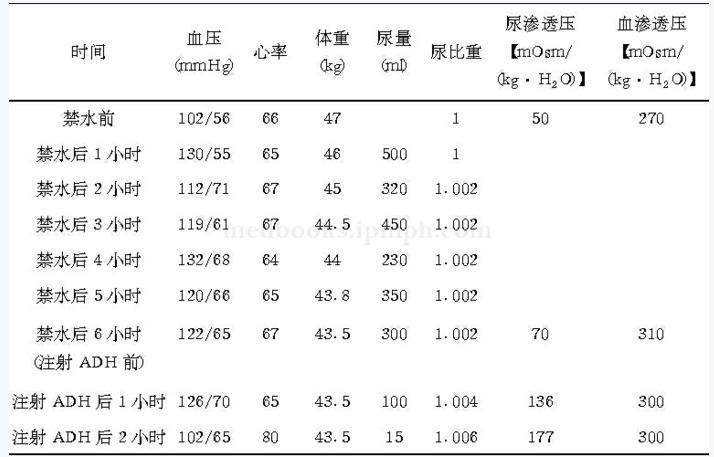
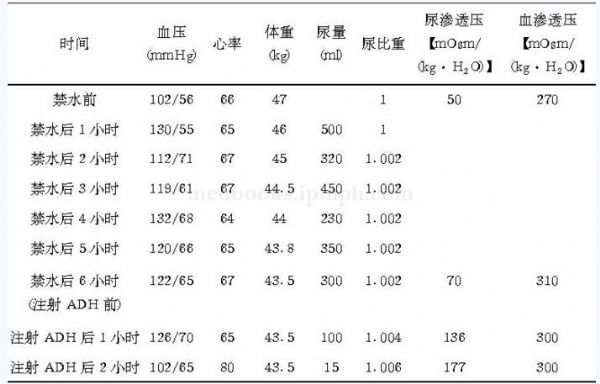
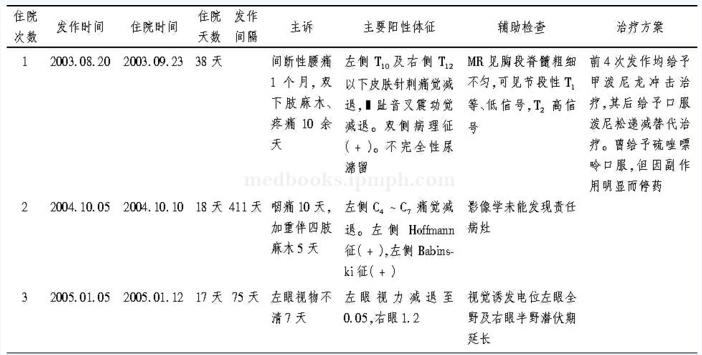
62岁女性,无明显诱因出现口干、多饮、多尿,尿量增多。以夜尿增多明显,10余次/晚,伴咽干、鼻干、纳差及体重下降等症状。经医生检查,发现并不是糖尿病所致。那到底是因何导致的呢?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#中枢性#
32
#完全性#
33
内分泌系统疾病.
52
好典型病例.学习了.
64
学习
64
学习了.谢谢.
68