Immunol Invest:IL-33基因多态性(Rs7044343)与过敏性鼻炎风险的相关性分析
2020-09-13 AlexYang MedSci原创
过敏性鼻炎(AR)是一种Th2介导的上呼吸道疾病,其中包括细胞因子基因在内的遗传因素起着重要作用。白细胞介素-33(IL-33)是初始T细胞极化为Th2表型的主要细胞因子,并能增强Th2细胞因子的分泌
过敏性鼻炎(AR)是一种Th2介导的上呼吸道疾病,其中包括细胞因子基因在内的遗传因素起着重要作用。白细胞介素-33(IL-33)是初始T细胞极化为Th2表型的主要细胞因子,并能增强Th2细胞因子的分泌。最近,有研究人员调查了IL-33单核苷酸多态性(SNPs)与IL-33血清水平与过敏性鼻炎的关系。

研究人员共收集了130名AR患者和130名健康个体的血液样本并对其进行了分析。统计学分析表明,TT基因型(OR=1.996,CI:1.168-3.412,P=0.01)和rs7044343 C > T的T等位基因(OR=0.675,CI:0.476-0.957,P=0.02)与AR风险降低显著相关。另外,与CC和CT基因型的受试者相比,携带TT基因型的个体IL-33水平更低;然而,这些差异没有统计学显著性。研究人员在rs1929992和rs12551256变体与AR风险之间也没有发现相关性,但rs1929992 A>G的GG基因型与对照组血清IL-33水平升高相关(P=0.01)。更多的是,AR患者和健康对照组之间的血清IL-33水平没有显著差异(p>0.05)。
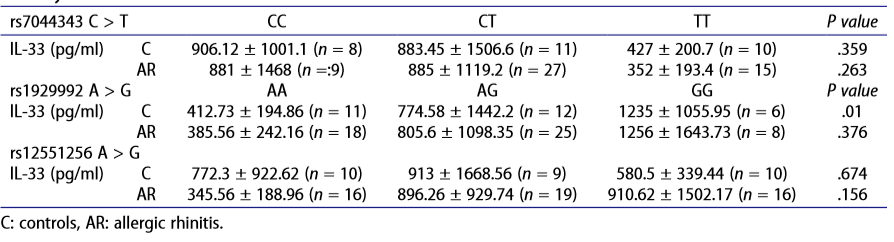
AR患者和健康对照中IL-33血清水平与3种不同IL-33 SNPs的相关性
最后,研究人员指出,rs7044343 C>T的TT基因型可能具有抗过敏性鼻炎的保护作用。
原始出处:
Sara Falahi, Seyed Hamid Reza Mortazavi, Farhad Salari et al. Association between IL-33 Gene Polymorphism (Rs7044343) and Risk of Allergic Rhinitis. Immunol Invest. Aug 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#过敏性#
36
#相关性#
34
#EST#
39
#IL-33#
35
#相关性分析#
0
#多态性#
37
学习
87
遗传因素对鼻炎的影响
88