AGING CELL:低血浆溶血磷脂酰胆碱与成人线粒体氧化能力受损有关
2019-02-10 海北 MedSci原创
随着年龄的增长,骨骼肌线粒体氧化能力的下降会对肌肉力量和身体表现产生不利影响。至今为止,与这种能力下降相关的因素尚未得到很好的表征。
随着年龄的增长,骨骼肌线粒体氧化能力的下降会对肌肉力量和身体表现产生不利影响。至今为止,与这种能力下降相关的因素尚未得到很好的表征。
低血浆溶血磷脂酰胆碱(LPC)是一类主要的全身生物活性脂质。已有的研究显示,其可预测衰老表型,如认知障碍和老年人步态速度的下降。
因此,最近,研究人员测试了低血浆LPC与受损的骨骼肌线粒体氧化能力相关的假设。
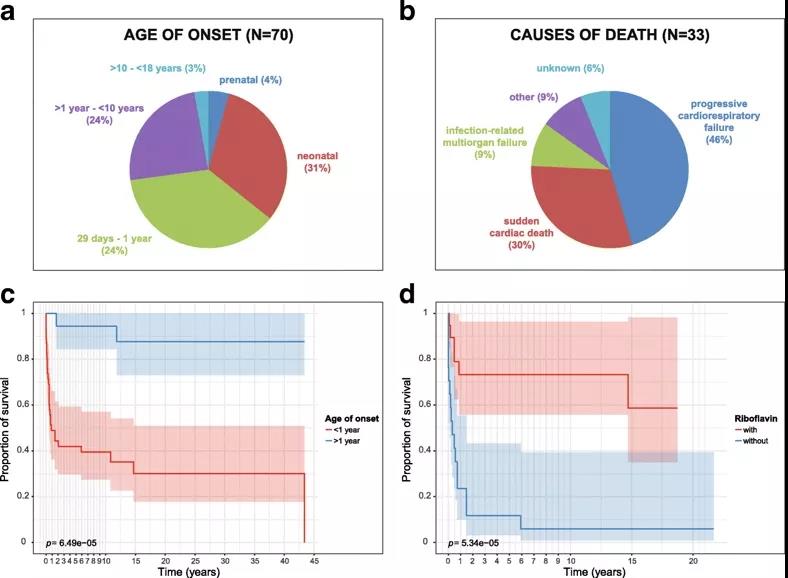
在巴尔的摩老年人纵向研究中,研究人员使用体内磷磁共振波谱(31P-MRS)测量385名参与者(256名女性,129名男性)的骨骼肌线粒体氧化能力,其年龄为24-97岁(平均72.5)。磷酸肌酸(PCr)的运动后恢复率kPCr被用作线粒体氧化能力的生物标志物。研究人员使用液相色谱 - 串联质谱法测量血浆LPC。
在多变量线性回归模型中调整了年龄,性别和身高后,与较低的三个四分位数相比较,kPCr最高四分位数的成人血浆具有更高的16:0(p = 0.04),16:1(p = 0.004),17:0(p = 0.01),18:1(p = 0.0002),18:2 (p = 0.002)和20:3(p = 0.0007)LPC,但不是18:0(p = 0.07),20:4(p = 0.09)LPC。
比较kPCr的下三个四分位数与最高四分位数的六个LPC,多个机器学习算法显示,接收器操作特征曲线下的面积为0.638(95%置信区间,0.554,0.723)。
因此,低血浆LPC与成人线粒体氧化能力受损有关。
原始出处:
Richard D. Semba et al. Low plasma lysophosphatidylcholines are associated with impaired mitochondrial oxidative capacity in adults in the Baltimore Longitudinal Study of Aging. Aging Cell, 2019; doi: https://doi.org/10.1111/acel.12915
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
32
#Cell#
35
#胆碱#
41
学习了,谢谢作者分享!
68
学习了谢谢分享
65