Cell:让你痛不欲生,让免疫系统束手就擒!哈佛华裔科学家破解病原菌劫持人体神经系统的阴谋
2018-05-21 BioTalker 奇点网
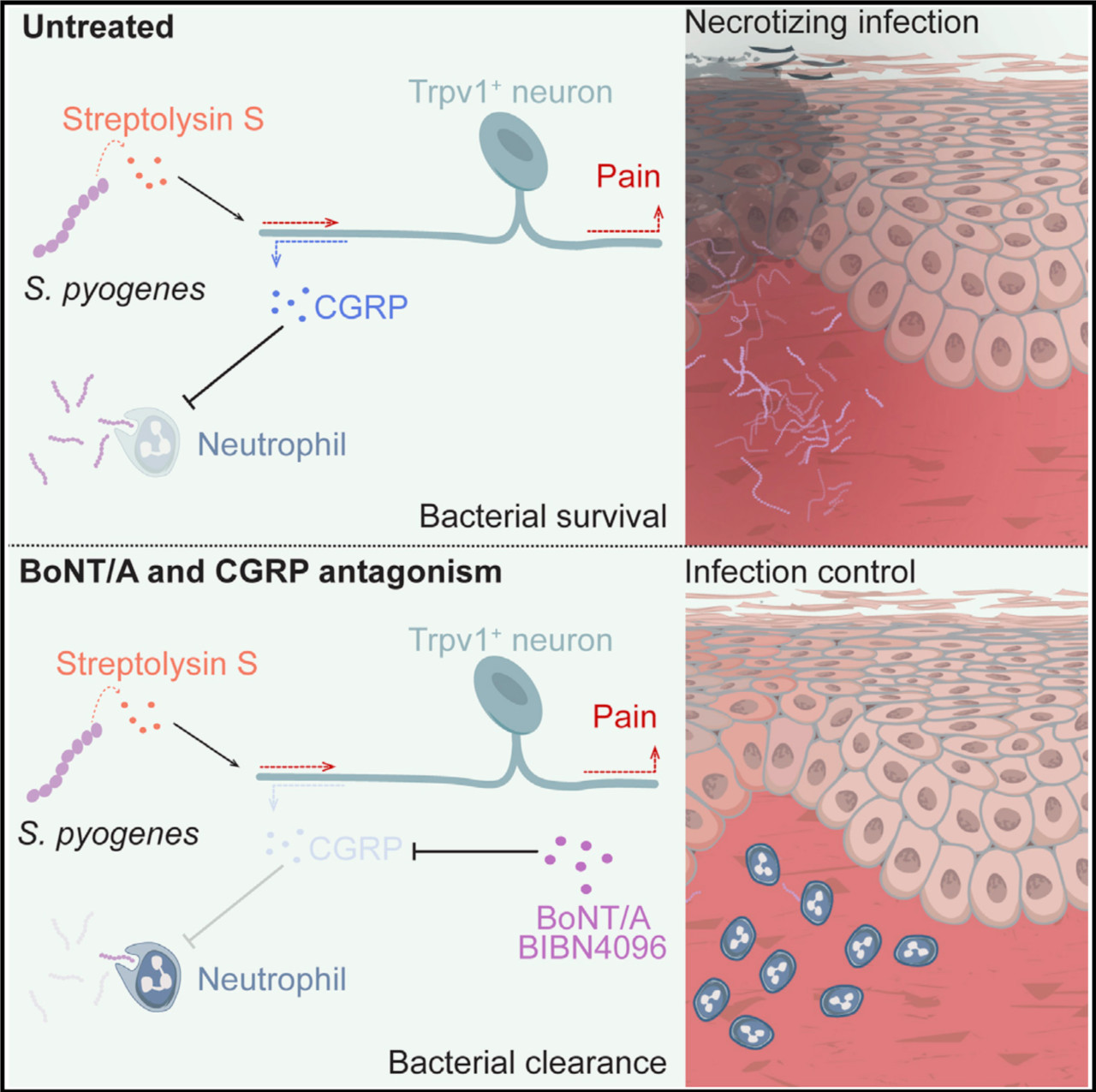
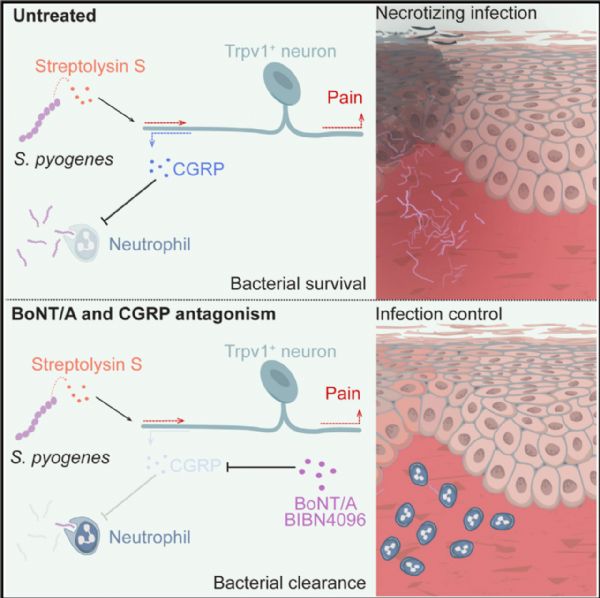
在很长的一段时间里,科学家认为,入侵的病原菌被人体免疫细胞识别,免疫细胞在召集更多免疫细胞的时候,还会激活周围的痛觉神经细胞[1]。痛觉神经细胞一边把一线的战况汇报给最高指挥部大脑,一边分泌一些信号分子,在一定程度上控制免疫细胞的活性,避免它们变得像绿巨人浩克那样杀敌八百自损三千。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#华裔#
48
#Cell#
37
#CEL#
36
免疫反应调节.
94
#病原菌#
30
#神经系统#
32
#哈佛#
29
学习了
72
一起学习学习
71
涨知识了
83