Front Oncol:呋喹替尼+PD-1抑制剂 vs 瑞戈非尼+ PD-1抑制剂治疗难治性微卫星稳定的转移性结直肠癌患者的疗效
2021-10-06 yd2015 MedSci原创
该研究表明,呋喹替尼+PD-1抑制剂(FP)可改善难治性微卫星稳定(MSS)的转移性结直肠癌患者的PFS。
结直肠癌全球发病率排名第三,死亡率排名第二。对于接受标准一线和二线治疗进展的晚期结直肠癌患者,三线治疗包括瑞戈非尼、呋喹替尼和TAS-102,但疗效一般。近年来,免疫检查点抑制剂(ICI)的应用为提高转移性CRC (mCRC)疗效带来了新的希望。但是,对于微卫星稳定(MSS)或无错配修复蛋白缺失(pMMR)的晚期结直肠癌患者,免疫检查点抑制剂(ICI)单药治疗无效。在一项II期临床研究,瑞戈非尼联合nivolumab治疗难治性mCRC(MSS或pMMR)的客观缓解率(ORR)为36%,中位无进展生存期(PFS)为7.9个月。因此,抗血管治疗联合PD-1抑制剂有可能改善患者的预后。近期,来自南昌大学的团队开展了相关研究,评估呋喹替尼+PD-1抑制剂(FP) vs 瑞戈非尼+ PD-1抑制剂(RP)治疗难治性微卫星稳定的转移性结直肠癌患者的疗效。相关结果发表在Frontiers in Oncology杂志上。

该研究回顾性收集2019年6月至2021年3月期间MSS或pMMR mCRC患者的数据。分析比较了FP和RP的疗效和安全性。
共51例患者纳入研究,其中FP方案治疗28例,RP方案治疗23例。接受FP或RP作为mCRC治疗的三线治疗的有56.9%,3线以上的有43.1%。39例(76.5%)为左半肿瘤,12例(23.5%)为右半肿瘤,38例(74.5%)有肝转移。原发肿瘤基因突变中,14例为RAS突变,1例为BRAF突变,18例为RAS/BRAF野生型。联合治疗中,呋喹替尼初始剂量分别为3mg(20例)、4mg(5例)、5mg(3例);至于瑞戈非尼, 17例患者开始服用80mg, 5例患者开始服用120mg, 1例患者开始服用160mg。使用的PD-1抑制剂类型有信迪利单抗(sintilimab), 卡瑞利珠单抗(camrelizumab), 特瑞普利单抗(toripalimab)和纳武利尤单抗(nivolumab)。FP组中使用PD-1抑制剂有sintilimab(53.6%)和camrelizumab (46.4%), RP组中camrelizumab(52.2%)是最常见的PD-1抑制剂。
全人群的ORR为7.8% (4/51),FP组的ORR为7.1% (2/28),而RP组ORR为8.7%(2/23)。FP组的DCR(89.3%)高于RP组(56.5%),全人群的DCR为74.5%。FP组获得疾病稳定(SD)的比例显著高于RP组(82.1% vs. 47.8%, P = 0.01)。
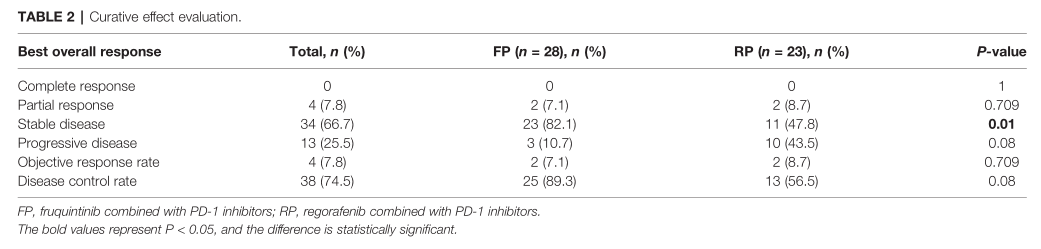
疗效评估
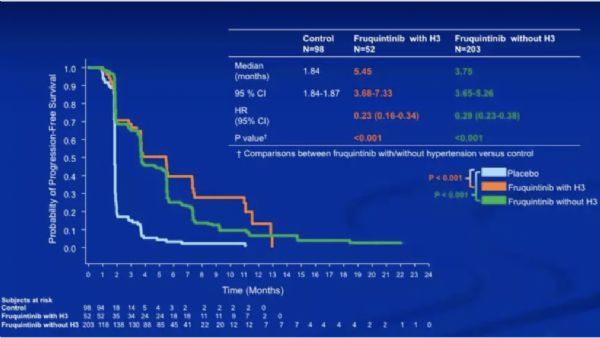
FP组的中位无进展生存期(PFS)为6.4个月(HR = 0.445;95% CI: 5.527-7.273), RP组3.9个月(HR = 0.594;95% CI: 2.736-5.064),差异有统计学意义(P = 0.0209)。

PFS
无肝转移患者中,FP组和RP组的中位无进展生存期(PFS)有显著差异(P<0.0001),但在肝转移患者中差异无统计学意义(P>0.05)。对于KRAS野生型患者,FP组和RP组之间的中位PFS有显著差异(P=0.0288)。对于KRAS突变患者,两组之间没有显著差异(P = 0.1836)。基于肿瘤的原发部位,左半结直肠癌患者FP组和RP组的中位PFS差异有统计学意义(P=0.0105),而右半结肠癌患者两组的中位PFS差异无统计学意义(P= 0.8538)。此外,FP组与RP组伴或不伴腹膜转移患者的中位无进展生存期(PFS)无显著差异(P >0.05)。
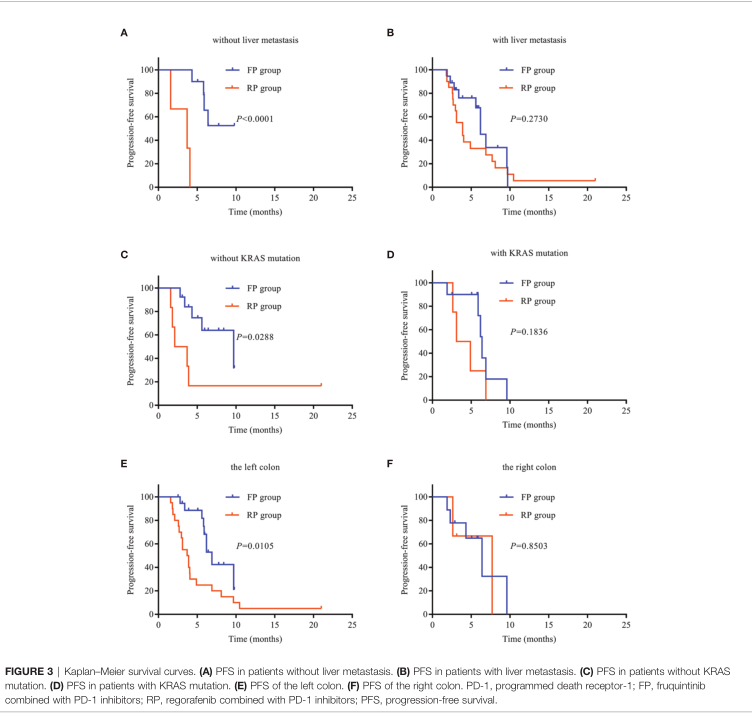
亚组分析PFS
对28例FP组患者和23例RP组患者的不良事件进行评估。所有患者都经历了不良事件。FP组任何级别的常见治疗相关不良事件(AE)为肝功能异常(42.8%)、手足综合征(39.3%)、高血压(35.7%)、毛细血管内皮增生(RCCEP)(39.3%)和蛋白尿(32.1%)。RP组中与治疗相关的任何级别的常见AE为肝功能异常(52.2%)、 手足综合征(43.5%)、高血压(39.1%)、RCCEP(39.1%)、蛋白尿(30.4%)和疲劳(30.4%)。RP组的肝功能异常、手足综合征和高血压发生率高于FP组,但差异无统计学意义。FP组的3级不良事件是腹泻(n = 1)和肝脏功能异常(n = 2);没有因不良事件而死亡。RP组3级不良事件为手足综合征(n = 1)、皮疹(n = 1)、肝功能异常(n = 1)、结肠穿孔(n = 1)、心肌酶升高(n = 1);一名患者死于免疫性心肌炎。
多因素分析显示,呋喹替尼对比瑞戈非尼的治疗方式是PFS的独立危险因素(HR = 2.688;95%CI:1.246 5.797;P = 0.012)。
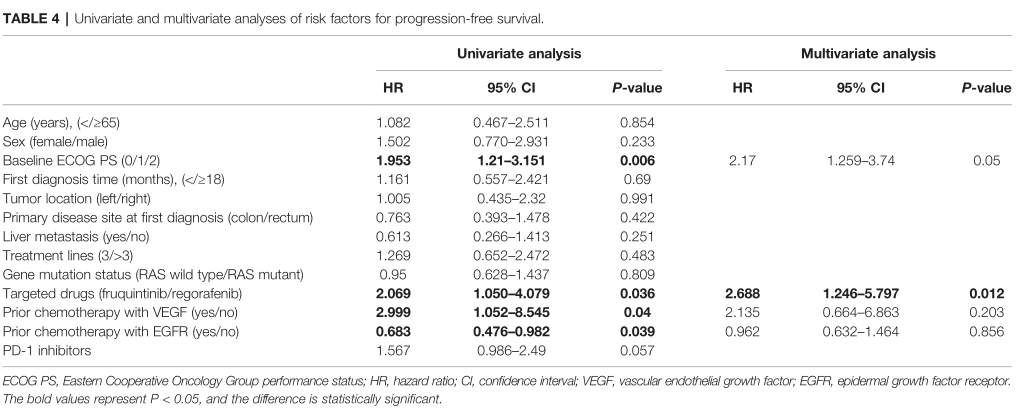
多因素PFS危险因素
综上,该研究表明,呋喹替尼+PD-1抑制剂(FP)可改善难治性微卫星稳定(MSS)的转移性结直肠癌患者的PFS。
原始出处:
Sun L, Huang S, Li D, Mao Y, Wang Y and Wu J (2021) Efficacy and Safety of Fruquintinib Plus PD-1 Inhibitors Versus Regorafenib Plus PD-1 Inhibitors in Refractory Microsatellite Stable Metastatic Colorectal Cancer. Front. Oncol. 11:754881.doi: 10.3389/fonc.2021.754881
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
49
#抑制剂#
38
#微卫星#
49
学习了
59
学习
52
瑞戈非尼联合nivolumab治疗难治性mCRC(MSS或pMMR)的客观缓解率(ORR)为36%,中位无进展生存期(PFS)为7.9个月。
62
#PD-1抑制剂#
39
#转移性#
32
#结直肠#
34
#难治性#
44