Stroke:动脉自旋标记灌注急性围产儿卒中的磁共振影像
2016-05-09 MedSci MedSci原创
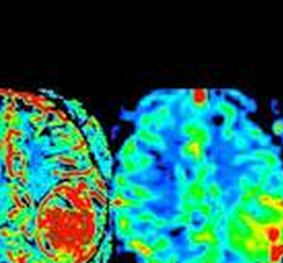
研究背景和目的:急性卒中成人的灌注加权的影像通常提示梗死核心及周边弥散受限的缺血半暗带的灌注减少。围产期卒中常见,但是其灌注模式很少提及。我们旨在描述发生围产期卒中新生儿的灌注模式。研究方法:有急性卒中临床特点的新生儿进行磁共振,使用连续的动脉自旋标记获得灌注数据。卒中定义为动脉性,静脉性及混合性,梗死核心通过在弥散加权成像表现为弥散受限获得。缺血区域的灌注加权图像和磁敏感加权图像,与对侧半球相应
研究背景和目的:急性卒中成人的灌注加权的影像通常提示梗死核心及周边弥散受限的缺血半暗带的灌注减少。围产期卒中常见,但是其灌注模式很少提及。我们旨在描述发生围产期卒中新生儿的灌注模式。
研究方法:有急性卒中临床特点的新生儿进行磁共振,使用连续的动脉自旋标记获得灌注数据。卒中定义为动脉性,静脉性及混合性,梗死核心通过在弥散加权成像表现为弥散受限获得。缺血区域的灌注加权图像和磁敏感加权图像,与对侧半球相应的区域对比。脑电图数据用于分析癫痫活动。
研究结果:在25例急性卒中的新生儿中,动脉缺血性梗死的11例中有8例,静脉性卒中的9例中有1例以及混合性的5例中的4例表现为高灌注。灌注不足在静脉性卒中的9例中看到3例,动脉性卒中中没有见到。21位病人的脑电图数据显示同侧半球的或癫痫电活动或局灶的尖波。
研究结论:在急性卒中的新生儿中获得的灌注加权图像常表现梗死核心高灌注。动脉性卒中的缺血半暗带很少发现。高灌可能是因为卒中后的再灌注或者卒中相关癫痫的神经元兴奋过度,这种认识可能对急性新生儿卒中的治疗的认识有帮助。
原始出处:
Watson CG1, Dehaes M1, Gagoski BA1, Grant PE1, Rivkin MJ2.et al,Arterial Spin Labeling Perfusion Magnetic Resonance Imaging Performed in Acute Perinatal Stroke Reveals Hyperperfusion Associated With Ischemic Injury.Stroke. 2016 May 3. pii: STROKEAHA.115.011936
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#动脉自旋标记#
43
好好看下
123
#磁共振#
43
很不错啊!
119