J Clin Invest:抗硬骨素单克隆抗体对HPP治疗的有效性及安全性评估
2017-04-28 MedSci MedSci原创
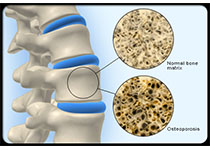
背景:低磷酸血症(HPP)是一种罕见的遗传性疾病,导致ALPL基因突变引起的骨形成和矿化的变化,编码组织非特异性碱性磷酸酶(ALP)酶。
背景:低磷酸血症(HPP)是一种罕见的遗传性疾病,导致ALPL基因突变引起的骨形成和矿化的变化,编码组织非特异性碱性磷酸酶(ALP)酶。
方法:在本阶段IIA开放标签,单中心,患者内,剂量递增的研究中,成年的低磷酸血症HPP患者分别在第1,15和29天接受3次静脉注射逐渐增加剂量(5,10和20mg / kg)的 BPS804(一种完全人类抗硬化蛋白单克隆抗体药物)。患者在最后一次用药后接受为期16周的随访,我们在治疗和随访期间以指定的间隔评估了BPS804给药的药效学,药代动力学,初步疗效和安全性。
结果:8名患者(平均年龄47.8岁)参加了研究(6名女性,2名男性)。 BPS804在第2天和第29天之间使平均ALP和骨特异性ALP酶活性增加。骨形成标志物前胶原I型N-末端前肽(PINP),骨钙素和甲状旁腺激素的瞬时增加以及观察到I型胶原的骨吸收标记C-端肽(CTX-1)。第85天和研究结束时显示腰椎骨密度平均增加。治疗过程中有轻度短暂的不良反应。
结论:BPS804治疗耐受性良好,导致骨形成生物标志物和骨矿物质密度增加,表明可以应用硬皮蛋白抑制来增强HPP成人非危及生命的临床情况下的骨矿物质密度,稳定性和再生。
原始出处:
Lothar Seefried, et al. Efficacy of anti-sclerostin monoclonal antibody BPS804 in adult patients with hypophosphatasia. J Clin Invest. doi:10.1172/JCI83731. Published April 24, 2017
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#克隆#
31
#EST#
31
学习了
52