Cell Rep:新研究发现促进小细胞肺癌发生发展和转移的重要分子
2016-07-10 佚名 生物谷
近日,来自荷兰癌症研究所的科研人员在国际学术期刊Cell Reports上发表了一项最新研究进展,他们在小细胞肺癌小鼠模型上找到了一种促进肿瘤发生和发展的重要转录因子,并且也在人类肿瘤样本中对该分子的表达情况与肿瘤进展之间的相关性进行了验证。该研究或为小细胞肺癌治疗和疾病进展诊断提供新的靶点和诊断标记。 小细胞肺癌(SCLC)是一种恶性的神经内分泌肿瘤,目前还没有文献报道找到有效的治疗
近日,来自荷兰癌症研究所的科研人员在国际学术期刊Cell Reports上发表了一项最新研究进展,他们在小细胞肺癌小鼠模型上找到了一种促进肿瘤发生和发展的重要转录因子,并且也在人类肿瘤样本中对该分子的表达情况与肿瘤进展之间的相关性进行了验证。该研究或为小细胞肺癌治疗和疾病进展诊断提供新的靶点和诊断标记。
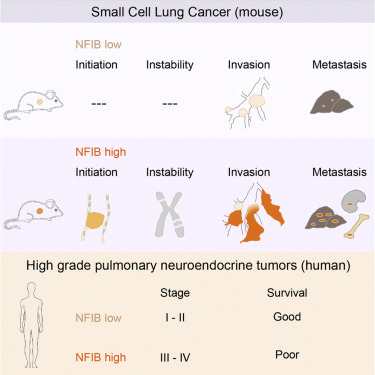
小细胞肺癌(SCLC)是一种恶性的神经内分泌肿瘤,目前还没有文献报道找到有效的治疗方法。该研究团队在之前研究中通过抑制Rb1和Trp53表达建立了SCLC小鼠模型,他们发现该小鼠经常出现Nfib和Mycl基因的异常表达。
在这项研究中,研究人员报告称虽然过表达上述任意一种转录因子都能够促进肿瘤生长,但是NFIB能够特异性的促进肿瘤的转移扩散。NFIB高表达水平与分化程度较低并且呈E-cadherin(CDH1)阴性的侵袭性肿瘤细胞群体的扩张性生长具有相关性。
与小鼠的研究数据一致,研究人员发现NFIB在几乎所有检测过的人类转移性高级别神经内分泌肺部肿瘤中都存在过表达,这提示NFIB或可成为临床检测肿瘤进展的一个标记物。
之前一些研究已经发现NFIB作为癌基因在三阴性乳腺癌,食管鳞状细胞癌以及下颌下腺癌等疾病中存在过表达,该研究进一步在小细胞肺癌中对NFIB的促癌作用进行了证明。这些结果都表明NFIB可能是癌症治疗和诊断的一个潜在靶点。
原始出处
Ekaterina A. Semenova1, 10, Min-chul Kwon1, 10, Kim Monkhorst2, 10.Transcription Factor NFIB Is a Driver of Small Cell Lung Cancer Progression in Mice and Marks Metastatic Disease in Patients.Cell Rep.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#研究发现#
31
#重要分子#
37
#CEL#
28
#发生发展#
43
#Cell#
25