Clin Gastroenterol H:肠道超声可用来监测克罗恩病
2016-11-30 haofan MedSci原创
在这项多中心前瞻性研究中,研究人员发现,超声检查可以用来监测活动性克罗恩病患者的疾病活动程度。肠道超声检查是评估疾病活动时早期透壁性变化的理想随访方法,以此来评价治疗疗效。
近日,消化病领域权威杂志Clinical Gastroenterology and Hepatology发表了一篇很有价值的研究文章,研究人员进行了一项多中心研究,旨在确定经腹肠壁超声,这种非侵入性的操作并且无需暴露于射线的检查方法是否可用于监测克罗恩病的病程进展。
研究人员在德国47个地区进行了一项为期12个月的前瞻性、非干预性研究,整个研究从2010年12月开始到2014年9月结束。在该研究中研究人员共纳入了234例经历过炎症发作的成年克罗恩病患者,即Harvey Bradshaw指数评分≥7分的患者。所有患者接受了强化治疗-主要用肿瘤坏死因子受体拮抗剂进行治疗。研究人员在研究之初、然后在进入研究的3个月、6个月和12个月时收集参与者的超声参数和临床数据并进行评估。主要终点事件为在纳入研究的12个月内超声参数的变化情况。
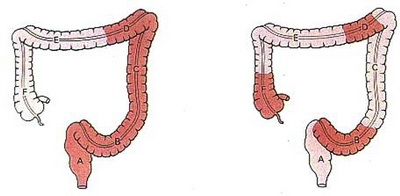
研究者发现,纳入研究的所有参与者均发生了肠壁的改变,主要发生在回肠末端和/或结肠段。在进入研究的第3个月和第12个月,超声检查显示几乎所有超声参数发生了显著的改善,包括肠壁增厚或分层减少,纤维脂肪细胞增殖降低,并且彩色超声多普勒信号增强(在进入研究的第3个月和第12个月所有参数均有P<0.01)。Harvey-Bradshaw指数评分的中位数从研究之初的10分经过12个月后下降到2分。在进入研究的第3个月后肠壁厚度的改善与C-反应蛋白水平降低有关(P≤0.001)。
由此可见,在这项多中心前瞻性研究中,超声检查可以用来监测活动性克罗恩病患者的疾病活动程度。肠道超声检查是评估疾病活动时早期透壁性变化的理想随访方法,以此来评价治疗疗效。
原始出处:
Torsten Kucharzik,et al. Use of Intestinal Ultrasound to Monitor Crohn’s Disease Activity. Clinical gastroenterology and hepatology. 2016.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#GAS#
26
#Gastroenterol#
17
#AST#
20
继续学习
33