Gastroenterology:10%的肿瘤性息肉可能未被完全切除
2013-01-06 Gastroenterology CMT
美国White River Junction退伍军人医疗中心的Heiko Pohl博士及其同事在《胃肠病学》(Gastroenterology)1月刊上报告称,在1,427例接受结肠镜检查的病例系列中,大约10%的直径介于5~20 mm的肿瘤性息肉未被完全切除。 在这项名为“完全腺瘤切除(CARE)”的研究中,Pohl博士及其同事对在这两家大型学术性医疗机构接受门诊结肠镜检查的年龄介于4
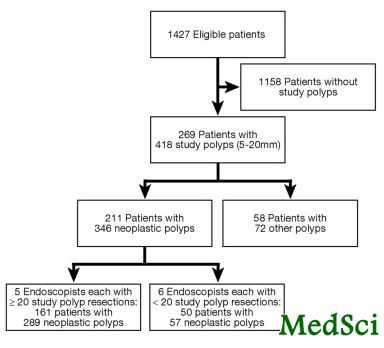
美国White River Junction退伍军人医疗中心的Heiko Pohl博士及其同事在《胃肠病学》(Gastroenterology)1月刊上报告称,在1,427例接受结肠镜检查的病例系列中,大约10%的直径介于5~20 mm的肿瘤性息肉未被完全切除。
在这项名为“完全腺瘤切除(CARE)”的研究中,Pohl博士及其同事对在这两家大型学术性医疗机构接受门诊结肠镜检查的年龄介于40~85岁的所有成年患者病例进行了分析,所有患者均无炎症性肠病病史,均不存在凝血功能障碍,并且检查示其至少存在1个直径介于5~20 mm的息肉。
参与这项研究的经过学会认证的胃肠病医生采用标准的结肠镜和息肉切除器以及标准的电刀工具来摘除病灶。胃肠病医生先测量并切除息肉,然后肉眼观察切缘,钳取切缘的活检样本,最后确认息肉已完全切除。医生还记录了整个切除操作是容易、比较困难还是困难。研究方案没有要求使用窄带成像或者氩离子血浆凝固术,但也允许各胃肠病医生视情况酌情使用。
由一名胃肠病理学专家独立分析所有残余腺瘤组织的活检样本并对息肉进行分类。共有346个(83%)息肉为肿瘤性。其中68%被归为管状、管状绒毛或者绒毛腺瘤。12%具有锯齿状组织学形态,包括42个 (10%)无蒂锯齿状腺瘤/息肉。
这名病理学专家发现,总的来看,大约有10%的肿瘤性息肉未被完全切除。大息肉(10~20 mm)不完全切除的几率比小息肉(5~9 mm)高1倍以上(17.3% vs. 6.8%)。无蒂锯齿状腺瘤/息肉不完全切除的几率比其他类型高3倍(31% vs. 7%)。因此,将近一半(48%)的无蒂锯齿状大腺瘤/息肉都未被完全切除。
Pohl博士及其同事写道:“由于腺瘤大小与晚期组织学病变的几率增加以及近期转变为癌症的风险增加相关,因此不完全切除体积较大的肿瘤性息肉是一个令人担忧的问题。”
研究没有发现与不完全切除相关的其他因素,包括切除操作被视为困难而非容易,息肉必须分块切除而非一次性切除,息肉位于右侧或左侧结肠以及息肉形态为扁平型或其他类型。
这346个肿瘤性息肉的切缘活检结果显示,35例患者的结肠内遗留了部分肿瘤性组织,共涉及这两家医疗中心的11名颇有经验的胃肠病医生。对于不同的内镜医生,不完全切除率差异很大,在6.5%~22.7%之间不等。而且,这些医生都知道他们在参与这项研究,可能在完成完全切除方面已经比平时更加谨慎。
Pohl博士及其同事说:“上述数据提示,在日常临床实践中息肉未被完全切除的现象可能比较常见,这可能与患者未来发生癌变有关。”研究结果还表明,目前结肠镜质量评价标准多以检出率为主,如今看来还应考虑切除的完全性。研究者指出:“高质量的有效的结肠镜操作不仅需要准确发现肿瘤性息肉,还需要完全切除这些息肉。”(Gastroenterology 2013;144:74-80)。
研究者说,到目前为止,“关于息肉切除是否充分的直接信息出乎意料的少。通常认为只要切除后肉眼没有发现任何明显的息肉组织,即可视为完全切除。采用带电刀的息肉切除器可能有助于进一步破坏残留的息肉组织”,但是否真能达到这样的效果,这还从未经过研究的证实。
研究者写道:“上述研究结果对息肉切除术的质量提出了质疑,呼吁大家需进一步完善肿瘤性息肉的切除,尤其是体积较大的息肉和无蒂锯齿状腺瘤/息肉。”此外,可能需要采用特殊的成像技术来评估息肉边缘,这一点应引起更多的关注。切除前勾画并标注息肉边缘也可能有助于提高息肉的完全切除率。对于部分病例,切除后辅以切缘消融处理可能也会有所帮助。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Gastroenterol#
41
#GAS#
53
好评
185
好评
157
#AST#
48
#Gastroenterology#
40