NEJM:预防卒中复发和心血管事件,替卡格雷的效果是否由于阿司匹林?
2016-07-08 MedSci MedSci原创
对于急性脑缺血患者来说,在预防复发性卒中和心血管事件的发生上,替卡格雷可能较阿司匹林的抗血小板治疗更有效。采用双盲对照试验,共纳入来自33个国家的674个中心的13199名非严重缺血性卒中或短暂性脑缺血发作的高危患者,且未接受过静脉或动脉内溶栓治疗,也并未患有心源性卒中。症状出现后24小时内按1:1的比例随机分配接受替卡格雷(6589名;第一天,180 mg;第2-90天,90毫克,每日两次)或阿
对于急性脑缺血患者来说,在预防卒中复发和心血管事件的发生上,替卡格雷可能较阿司匹林的抗血小板治疗更有效。
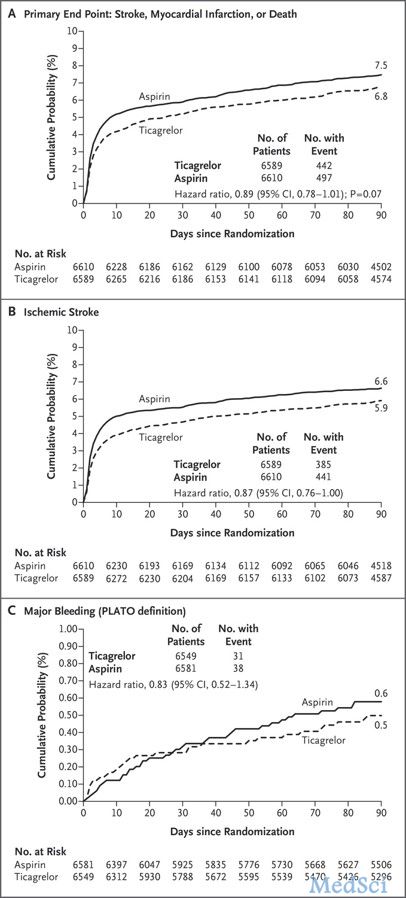
采用双盲对照试验,共纳入来自33个国家的674个中心的13199名非严重缺血性卒中或短暂性脑缺血发作的高危患者,且未接受过静脉或动脉内溶栓治疗,也并未患有心源性卒中。症状出现后24小时内按1:1的比例随机分配接受替卡格雷(6589名;第一天,180 mg;第2-90天,90毫克,每日两次)或阿司匹林(6610名;第一天,300毫克;第2-90天,每日100毫克)治疗。主要终点为90天内发生中风、心肌梗死或死亡的时间。
结果,在90天的治疗期间,替卡格雷治疗组共有442名(6.7%)患者发生主要终点事件,阿司匹林治疗组共有497名 (7.5%)患者发生主要终点事件(风险比,0.89;95% CI,0.78-1.01;P = 0.07)。385名(5.8%)经替卡格雷治疗的患者,及441名(6.7%)经阿司匹林治疗的患者发生缺血性脑卒中(风险比,0.87;95% CI,0.76 - 1)。0.5%经替卡格雷治疗的患者和0.6%经阿司匹林治疗的患者发生大出血,颅内出血的比例分别为0.2%和0.3%,发生致命性出血的比例均为0.1%。
总而言之,该研究发现,对于急性缺血性卒中或短暂性脑缺血发作的患者来说,在降低其90天内卒中、心肌梗塞或死亡发生率上,替卡格雷的治疗效果并不优于阿司匹林。
原始出处:
S. Claiborne Johnston, et al., Ticagrelor versus Aspirin in Acute Stroke or Transient Ischemic Attack. N Engl J Med 2016; 375:35-43July 7, 2016DOI: 10.1056/NEJMoa1603060.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#血管事件#
41
谢谢分享谢谢指点
65
好文值得点赞!继续关注学习。
64
继续关注中
97
有时候可以联合应用
131
新药使用时应该慎重解释临床试验结果
92
#替卡格雷#
30
#卒中复发#
43
这是一个阴性结果,表明并不比阿司匹林更好。
57
有时候我们不能过于迷信一些新药,需要规范的临床研究进行验证,往往有些老药功效其实是非常不错
70