Thorax:6岁前吸入皮质类固醇治疗与身高和骨密度的关系
2022-02-01 MedSci原创 MedSci原创
儿童早期使用ICS与6岁时身高降低有关,但仅适用于在6岁时仍继续ICS治疗的儿童。
吸入性皮质类固醇是治疗儿童哮喘的首选控制疗法,但之一疗法具有潜在的副作用。婴幼儿可能特别容易受到吸入性皮质类固醇的潜在副作用的影响,其对身高和骨矿物质含量(BMC)具有不良影响。吸入性皮质类固醇抑制生长的风险可能在1-6岁的婴儿和年幼儿童中尤其明显,因为该年龄组的儿童生长速度快,但在长期前瞻性研究中很少对此进行研究。

近日,胸部疾病领域权威杂志Thorax上发表了一篇研究文章,研究人员纳入两项哥本哈根儿童哮喘前瞻性研究队列中的儿童。研究人员从儿童出生到6岁进行前瞻性登记中心获取吸入性皮质类固醇的使用情况,并计算累积剂量。该研究的主要结果是6岁时双能X射线吸收测定(DXA)扫描的身高和BMC。

在6岁时,队列中共有930名儿童(84%)进行了有效的身高测量,792名儿童(71%)进行了DXA扫描。291名儿童(31%)在6岁前接受了相当于或超过10周标准治疗的累积吸入性皮质类固醇剂量。
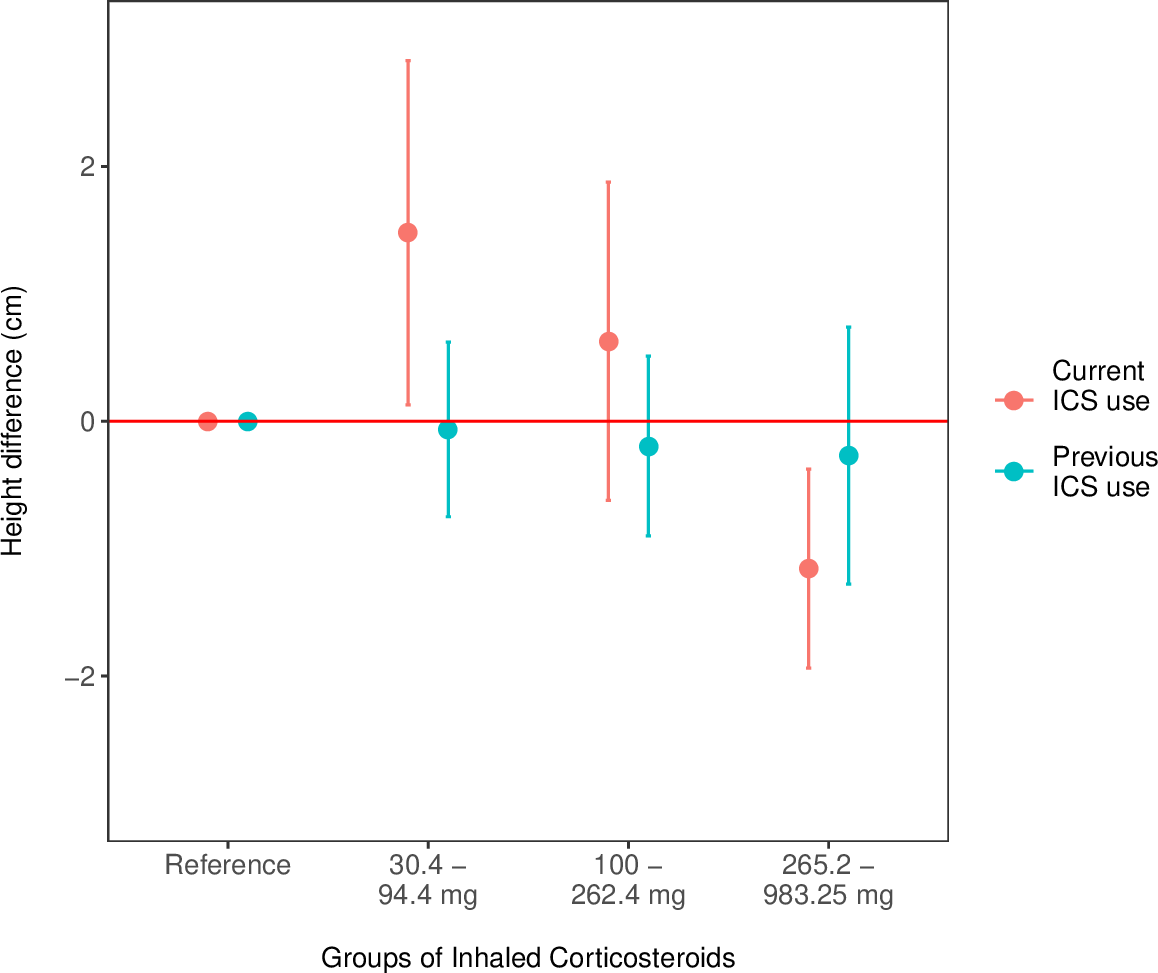
研究人员发现吸入性皮质类固醇的使用与儿童身高呈负相关,0至6岁的儿童接受1年的标准治疗身高降低0.26cm(95%CI为-0.45至-0.07),p=0.006。这种影响主要是由5至6岁之间持续治疗的儿童所驱使的(-0.31cm(95%CI为-0.52至-0.1),p=0.004),而6岁前至少停止吸入性皮质类固醇治疗1年的儿童没有显著相关性(-0.09cm(95%CI为-0.46至0.28),p=0.64)。6岁时使用吸入性皮质类固醇治疗与BMC之间没有关联。
由此可见,儿童早期使用吸入性皮质类固醇与6岁时身高降低有关,但仅适用于在6岁时仍继续采用吸入性皮质类固醇治疗的儿童。
原始出处:
Asja Kunøe,et al.Height and bone mineral content after inhaled corticosteroid use in the first 6 years of life.Thorax.2022.https://thorax.bmj.com/content/early/2022/01/19/thoraxjnl-2020-216755
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
40
好文章
45
继续学习
44
#类固醇#
0