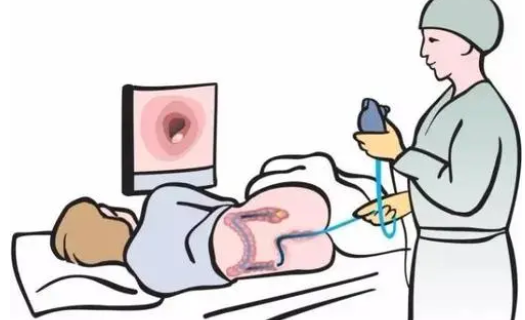
结直肠癌(CRC)是一种常见的致命疾病。筛查能提供获益,因为切除早期腺瘤可以预防CRC,切除局限性癌症或许能预防CRC相关性死亡。CRC在40岁前并不常见;40岁后,发病率逐渐上升,到80岁时达到每年3.7/1000。美国一般风险患者的CRC终生发病率为4.5%,其中90%的病例发生在50岁以后。
在世界范围内,CRC是女性中第二常见、男性中第三常见的癌症,在2012年造成了69多万例死亡。在美国,CRC是癌症死亡的第二大病因,CRC引起的死亡约占总体癌症死亡的8.4%。大约每3例CRC患者中有1例会因此死亡。
有一个令人欣慰的现象便是,最近几年来,大家普遍认识到筛查是预防CRC一个十分重要的措施。在2004-2013年间,CRC的死亡率平均每年下降2.7%。微观模拟模型MISCAN-Colon提示,所观察到的CRC死亡率下降,可能约有53%得益于CRC筛查。一项有关美国CRC发病率和筛查率的时间趋势的研究报道,从1987-2010年,约25-50万例CRC病例可能通过筛查得到了预防,同时发现的CRC由晚期向早期疾病转变。
目前,欧洲各国的结直肠癌筛查方案和接受情况有很大的不同。在许多高收入国家,结肠直肠癌的总体发病率正在下降,然而在美国和其他高收入国家,如澳大利亚、加拿大和挪威的分析表明,50岁以下的成年人的发病率正在上升。
那么不同国家大肠癌发病率、死亡率和分期分布随时间的变化如何呢?为了讨论上述问题,国际癌症研究机构对7个发达国家进行了跨国研究,结果发表在Lancet Gastroenterology & Hepatology杂志上。
研究人员从澳大利亚、加拿大、丹麦、挪威、新西兰、爱尔兰和英国的20个以人口为基础的癌症登记处获得了结肠癌和直肠癌的发病率数据,使用年龄-时期-队列模型来评估各年龄组、时期和出生队列的发病率趋势。

7个国家不同年龄段年龄标准化的发病率
所有研究国家都注意到结肠癌和直肠癌发病率的总体下降或稳定。然而,在有数据可查的最近10年期间,丹麦(每年3.1%)、新西兰(每年2.9%)、澳大利亚(每年2.9%)和英国(每年1.8%)50岁以下人群的结肠癌发病率显著上升。在加拿大(每年3.4%)、澳大利亚(每年2.6%)和英国(每年1.4%),这一年龄组的直肠癌发病率的年平均百分比变化也有明显的增加。
同时,在50-74岁的人群中,结肠癌发病率的年平均百分比变化在澳大利亚(每年1.6%)、加拿大(每年1.9%)和新西兰(每年3.4%)显著下降,直肠癌的发病率在澳大利亚(每年2.4%)、加拿大(每年1.2%)和英国(每年1.2%)显著下降。

7个国家50岁以下年龄段年龄标准化的发病率
此外,50岁以下人群结直肠癌发病率的增加主要是由结肠远端(左侧)肿瘤的增加引起的。在所有国家,使用非线性队列效应,直肠癌比结肠癌更明显。
综上,本研究7个国家中50岁以下人群的结直肠癌发病率大幅增加。
参考文献:
Changes in colorectal cancer incidence in seven high-income countries: a population-based study. DOI:https://doi.org/10.1016/S2468-1253(19)30147-5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#发病率#
44
#研究机构#
56
#癌发病#
50
#癌发病率#
50
#结直肠#
51
#癌症研究#
43