Obstet Gynecol:骨盆重建手术后需要限制活动吗?
2017-04-03 xing.T MedSci原创
脱垂手术后3个月,自由活动组女性与建议限制术后活动的妇女相比满意度同样高。术后自由活动的妇女脱垂和尿道症状较少,并且具有相似的短期解剖结局,表明允许妇女术后恢复正常活动可能改善盆底结局。
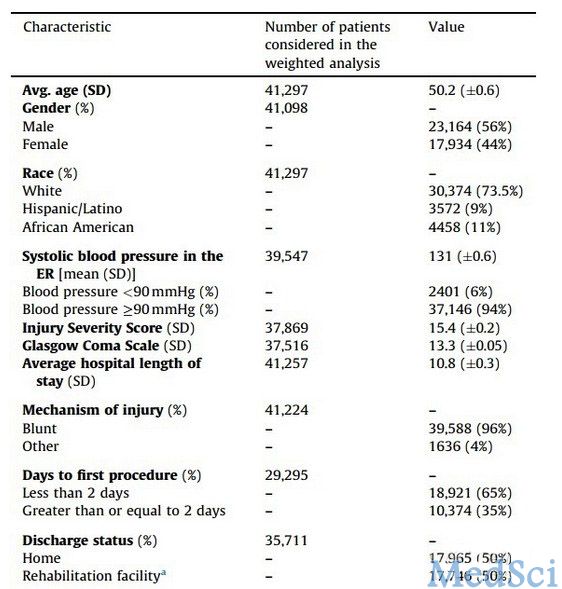
在这项多中心、随机、双盲的临床试验中,接受脱垂重建手术的妇女术后随机分为自由活动组与建议限制性术后活动组。自由活动建议指导妇女术后活动按照自身的节奏进行,对于提升或高强度运动没有限制。相反,限制性建议指导妇女避免3个月内进行重力提升或剧烈运动。该研究的主要结局是患者满意度,是通过术后3个月采用5分Likert量表的问题“您对脱垂手术的结果如何满意?”进行评估。次要结局包括解剖结局和盆底症状。
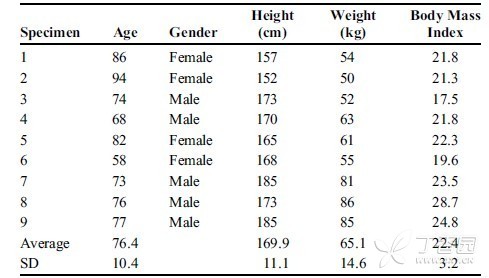
从2014年9月至2015年12月,共筛选了130名妇女,其中108人被随机分配。最终,95人被分为两组进行干预。(n=45自由活动,n=50限制活动),并完成主要结局评估。基线特征(包括盆腔器官脱垂程度和人口统计学特征)和手术干预情况在两组间无差异。大多数妇女接受了侵入性阴道骶骨缝合术(58例),其次为阴道悬吊术(27例)或阴道封闭术(9例)。自由活动组和限制性活动组的满意度一样高(98% vs. 94%,比值比为0.36 [0.036-3.55],P=0.619)。 解剖结局在组间没有差异; 然而,自由活动组中报告的盆底症状较少。
脱垂手术后3个月,自由活动组女性与建议限制术后活动的妇女相比满意度同样高。术后自由活动的妇女脱垂和尿道症状较少,并且具有相似的短期解剖结局,表明允许妇女术后恢复正常活动可能改善盆底结局。
原始出处:
Mueller, Margaret G, et al. Activity Restriction Recommendations and Outcomes After Reconstructive Pelvic Surgery: A Randomized Controlled Trial.Obstetrics & Gynecology.2017.http://journals.lww.com/greenjournal/Fulltext/2017/04000/Activity_Restriction_Recommendations_and_Outcomes.3.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TET#
40
#NEC#
37
学习过了,分享!
55
学习了很有用
71
学习了
80