JAMA:Aleglitazar不减少2型糖尿病患者ACS后心血管风险
2014-04-04 佚名 dxy
糖尿病促进动脉粥样硬化的发生发展,从而增加心血管事件风险。针对心血管传统危险因素的治疗手段有效减少糖尿病或非糖尿病患者的心血管风险,但是没有缓解与糖尿病相关的额外风险。目前尚无研究明确表明糖尿病特异性治疗药物或严格控制血糖可以减少糖尿病大血管事件发生。【原文下载】 为此,来自美国克利夫兰临床中心的Lincoff教授等进行了一项名为AleCardio的研究,旨在研究标准方案治疗基础上增加Ale
糖尿病促进动脉粥样硬化的发生发展,从而增加心血管事件风险。针对心血管传统危险因素的治疗手段有效减少糖尿病或非糖尿病患者的心血管风险,但是没有缓解与糖尿病相关的额外风险。目前尚无研究明确表明糖尿病特异性治疗药物或严格控制血糖可以减少糖尿病大血管事件发生。【原文下载】
为此,来自美国克利夫兰临床中心的Lincoff教授等进行了一项名为AleCardio的研究,旨在研究标准方案治疗基础上增加Aleglitazar(一种强有力的过氧化物酶体增殖物激活受体PPARα/γ双激动剂)是否减少近期发生急性冠脉综合症(ACS)的2型糖尿病患者的心血管死亡及发病风险。
研究发现Aleglitazar不减少近期发生ACS的2型糖尿病患者心血管事件风险,研究结果发表在2014年3月30日的JAMA杂志上。
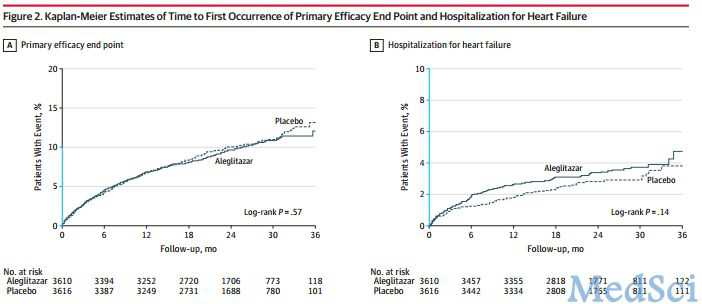
AleCardio研究共纳入7226名在2010年2月和2012年5月期间发生ACS(心肌梗死或不稳定型心绞痛)的2型糖尿病患者。患者按1:1随机分为aleglitazar组(150ug,1/日)或安慰剂组,至少随访2.5年。研究主要终点事件心血管死亡、非致命性心梗或非致命性卒中,主要安全终点为因心衰住院和肾功能损害。
研究结果表明,Aleglitazar组和对照组主要终点事件发生率分别为9.5%和10.0%.Aleglitazar组患者心衰、胃肠道出血和肾功能不全等严重不良事件发生率增加(分别为3.4%VS2.8%、2.4%VS1.7%和7.4%VS2.7%)。该研究也因无效且增加不良事件而于2013年6月2日终止。
研究发现Aleglitazar不减少近期发生ACS的2型糖尿病患者心血管事件风险。
编后记:过氧化物酶体增殖物激活受体(PPARs)起着调节脂质和能量代谢基因的作用。PPAR-α激动剂贝特类降脂药降低血清甘油三酯,而PPAR-γ激动剂噻唑烷二酮类降糖药降低血糖,增加胰岛素敏感性。由于糖尿病患者动脉粥样硬化与血脂紊乱和胰岛素抵抗有关,因此PPAR-α/γ双激动剂可能在调节血脂的同时改善胰岛素抵抗。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#AZ#
43
#血管风险#
36
#ACS#
36
#2型糖尿病患者#
32
#糖尿病患者#
25