Cardiology:每天饮用能量饮料超过2杯,会增加心血管疾病风险
2016-02-04 QQduhp 译 MedSci原创
CDC的数据显示,约31%12-17岁青少年经常饮用能量饮料,34%18-24岁青年人定期饮用添加有兴奋剂的能量饮料。 阿德莱德大学的药理学博士Ian Musgrave指出,在过去的十年里能量饮料普遍受到民众欢迎,民众希望借此减轻疲劳,减少困意并提高注意力。他和同事将研究成果发表在在Cardiology。 虽然含有咖啡因的能量饮料较多,但其中也可含有植物性兴奋剂、单糖和其他添加剂等。 为了深入调查
CDC的数据显示,约31%的12-17岁青少年经常饮用能量饮料,34%的18-24岁青年人定期饮用添加有兴奋物质的能量饮料。
阿德莱德大学的药理学博士Ian Musgrave指出,在过去的十年里能量饮料普遍受到民众欢迎,民众希望借此减轻疲劳,减少困意并提高注意力。他和同事将研究成果发表在在Cardiology。
虽然含有咖啡因的能量饮料较多,但其中也可含有植物性兴奋物质、单糖和其他添加剂等。
为了深入调查和观察能量饮料对民众的影响,研究人员对2014-2015年间因心悸问题就诊于南澳大利亚医院急诊科的患者进行了探究。
研究人员指出,就诊急诊的患者中约70%的患者曾饮用过某种类型的能量饮料。
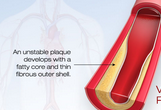
研究人员发现一个更直接的联系:在受访患者中,36%的就诊患者在饮用能量饮料后24小时内去急诊就诊。这些患者中,有8位患者饮用能量饮料超过5种,1人饮用12种能量饮料,同时还饮酒。此外,他们发现,相比饮用能量饮料少于1杯/天的民众,饮用能量饮料更多的民众发生心悸的风险及频率更高。研究人员还指出,对于健康且无心脏病高危风险因素的民众而言,饮用能量饮料后可出现心率加快、心悸、胸痛等症状。
Musgrave博士认为,学者们越来越担心含咖啡因的酒精饮料(CABs)对机体有害。2010年11月,FDA就曾强制要求7种CABs饮料退出销售市场。
Musgrave博士补充道:“含有酒精的饮料对人们的危害在于,它不仅削弱人们的思考和决断能力,同时也减慢能量饮料中咖啡因的分解代谢速度。”
他认为,尽管咖啡因是最安全的兴奋剂之一,但摄入含咖啡因的饮料会增加民众患心脏病的风险。这项研究有助于遏制民众无节制饮用能量饮料,推荐摄入量的最大剂量为2杯/天。
原始出处:
Scott Willoughby et al.A survey of energy drink consumption among young patients presenting to the emergency department with the symptom of palpitations,International Journal of Cardiology, 1 Feb,2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cardiology#
34
#Cardiol#
31
学习了,谢谢。
125
#疾病风险#
38
#血管疾病#
39
#能量饮料#
35
赞
71
个性化
120
应该是。做的好,定量化
154