15块钱小苏打治肝癌,什么情况?
2016-09-23 熊坨坨 “医学界”微信号
昨天,一则某大众媒体的医学报道突然火了——真是这么回事吗?让我们来看看原研究怎么说的吧……先上个论文摘要由于这次媒体报道实在太玄乎,咱们还是来看看朴实无华的原文摘要,先来搞清一下是怎么回事。首先呢作者说因为之前的其他研究有提示中和肿瘤内如酸中毒和葡萄糖剥夺联合起来可以产生控制肿瘤的效果。所以他们进行了两个临床试验,一个是随机的(样本为20名大肝癌患者),另一个不是(样本为57名大肝癌患者)。采取的
昨天,一则某大众媒体的医学报道突然火了——

真是这么回事吗?
让我们来看看原研究怎么说的吧……
先上个论文摘要
由于这次媒体报道实在太玄乎,咱们还是来看看朴实无华的原文摘要,先来搞清一下是怎么回事。
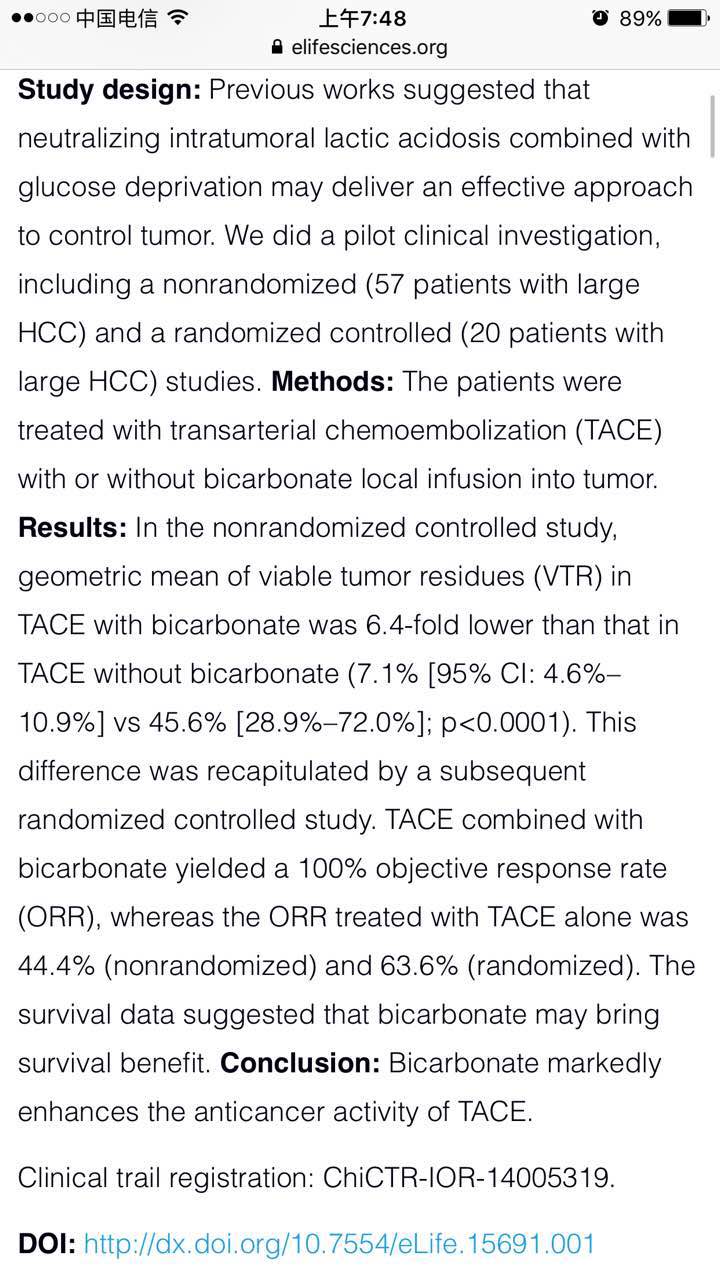
首先呢作者说因为之前的其他研究有提示中和肿瘤内如酸中毒和葡萄糖剥夺联合起来可以产生控制肿瘤的效果。所以他们进行了两个临床试验,一个是随机的(样本为20名大肝癌患者),另一个不是(样本为57名大肝癌患者)。
采取的方式是给患者做TACE(经动脉化疗栓塞术),然后一部分人同时使用重碳酸盐局部灌注肿瘤,其余人不用。
他们得到的结果就是额外使用重碳酸盐局部关注的患者效果优于没有使用的。
具体好多少呢?
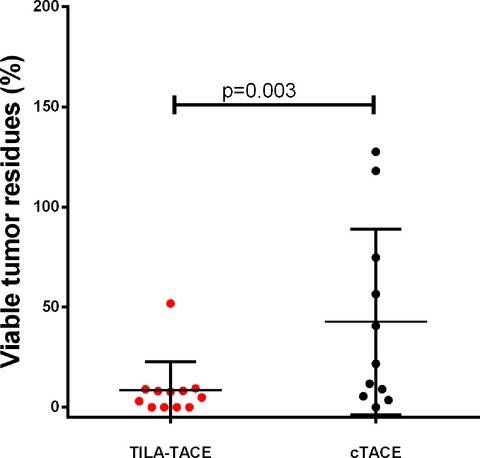
这是随机对照试验组的结果,Y轴代表肿瘤残余的占比,左边为使用重碳酸盐冲洗的患者,右边是不使用的。很明显,试验组比对照组的肿瘤残余比例更小。
数据分析得,TILA-TACE组比对照组进步了80.1%。

在肿瘤对治疗的反应上,对照组也优于cTACE组。试验组TILA-TACE有更多的完全反映(CR),达到了33.3%,而对照组仅有9.1%。
生存期才是硬道理
检验肿瘤治疗效果的标准当中,生存期应该是绕不过去的。那么,TILA-TACE与对照组比,在生存期上有什么进展?
1)在非随机队列研究中,对比如下——
生存率 | TILA-TACE | cTACE |
1年生存率 | 82.8% | 66.7% |
2年生存率 | 67.7% | 40.7% |
3年生存率 | 61.8% | 25.9% |
TILA-TACE治疗的患者中位生存期为41个月,cTACE为14个月。
在非随机对照试验当中,这个结果看上去很不错,中位生存期有了极大的提高。
2)那在随机对照试验中,结果怎样呢?
比较遗憾的是,由于样本量发生变动,随机对照试验的结果显示两者没有生存期上的明显差异。
TILA-TACE组3人死亡,7人存活。
cTACE组6人中3人死亡,剩下4人由于中途更换治疗方案为TILA-TACE。
有没有问题呢?
实际上网上放出的原文中还真有三个修正问题。
第一个问题问的是为什么没有更加详细的操作方案以便其他人进行重复试验。研究者随后给出了具体方案。
第二个问题质问为什么没有给对照组使用用作安慰剂的生理盐水进行灌注以对应使用中碳酸盐的TILA-TACE组。研究者给的答复是生理盐水会影响cTACE的效果,也就是说对照组确实没有被给予安慰剂……
第三个问题则是问为什么对照组的中位生存期这么低,因为14个月远低于cTACE应有的生存期以及各指南当中给出的平均生存期。研究者的回答是考虑到对照组患者的疾病特征,比如BCLC阶段和肿瘤体积,这个生存期并不低……
好吧。
TACE是个新玩意儿嘛?
不是。
经导管肝动脉化疗栓塞(TACE)被日本人山田提出并且实践,已经是上世纪70年代的事儿了。1978年山田教授提出TACE之后,自己也进行了各种实践,最终这种方法被学界认可。
简单来说,TACE是现在肿瘤介入治疗的重要手段,也是应用非常广泛的手段。
要用更简单一点的话解释TACE的话,就是这位摘录的这段当中的后半句——
“堵上血管,断了补给”,就是TACE的作用。
简单来说,这项研究就是在已经成熟的TACE上进行进一步的试验改良。因为TACE是这个试验改良的基础,所以价格只可能更高,不可能更低,某些媒体传“降低肝癌治疗价格”也不知道依据是啥……
实际上,在TACE基础上进行改良的研究非常多,适逢CSCO大会召开,也听了几场肝癌的会,来自香港的肝肿瘤介入专家Thomas Wai- Tong Leung就介绍了TACE的其他改进方式——

CSCO现场,肝癌论坛,香港专家正在介绍DEB TACE
会后,询问这位介入专家,对浙江这项今年8月2日发表,在昨晚突然轰动起来的研究有什么看法。专家表示没有听过。详细介绍论文内容之后,专家表示不发表评论。
参考文献:
Chao M, Wu H, Jin K, Li B, Wu J, Zhang G, Yang G, Hu X. A nonrandomized cohort and a randomized study of local control of large hepatocarcinoma by targeting intratumoral lactic acidosis. Elife. 2016 Aug 2;5. pii: e15691. doi: 10.7554/eLife.15691.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














怀疑真实性!
85
很好,很有帮助,应该大力投资研发这样的研究,造福人类社会,帮助其他患者,早日康复
78
很好,很有帮助,应该大力投资研发这样的研究,造福人类社会,帮助其他患者,早日康复
75
#小苏打#
36
嘿嘿呵呵无语可能在临床有应用这个药物
66
继续关注
62
第一个问题问的是为什么没有更加详细的操作方案以便其他人进行重复试验!!!
31
这个结果看上去很不错,中位生存期有了极大的提高!!!
30
总结的很好~!!
25
总结的很好!!!
26