J Thorac Oncol: Capmatinib治疗既往应用过MET抑制剂的肺癌的疗效:一项II期临床试验
2021-05-15 yd2015 MedSci原创
伴有MET基因改变的肺癌患者克唑替尼(crizotinib)治疗后再用Capmatinib治疗仍有中等疗效,可能归功于交叉的耐药机制。
Capmatinib是一种高度选择性和有效的MET-TKI抑制剂,具有强大的中枢神经系统(CNS)穿透能力。美国FDA已经批准Capmatinib治疗含有MET第14外显子跳跃改变的非小细胞肺癌(NSCLC)。在II期临床试验 GEOMETRY Mono-1中试验中,Capmatinib治疗接受过化疗的MET 14外显子改变的非小细胞肺癌患者客观缓解率(ORR)为41%,而没有接受过治疗的患者ORR为68%。Capmatinib的颅内控制率为54%。除了Capmatinib,临床上也有相应的MET-TKI抑制剂,包括克唑替尼(crizotinib), tepotinib 和savolitinib。但是,一种MET抑制剂失败后,再用一种高选择颅内穿透性的MET抑制剂,是否还有较高的疗效。因此,国外学者开展了一项II期临床试验,评估MET抑制剂治疗伴有MET扩增或14外显子跳跃突变的NSCLC失败后,接着应用Capmatinib的疗效。相关研究结果发表在J Thorac Oncol杂志上。
这是一项开放标签、研究者发起的单中心、单臂的II期临床试验。纳入标准:年龄大于等于18岁,IIIB至IV期MET扩增或14外显子跳跃突变的NSCLC,脑转移患者无神经症状以及无需激素治疗可纳入,既往接受过MET抑制剂治疗,也包括没有治疗过的患者。MET基因经过二代测序检测确认。纳入患者接受capmatinib 400 mg/bid,主要研究终点为客观缓解率(ORR)。次要终点为无进展生存期(PFS),疾病控制率 (DCR), 总生存期(OS)。循环肿瘤DNA(ctDNA)被用来鉴定capmatinib的耐药机制。
从2016年5月至2019年11月,共20例患者纳入研究,其中15例患者伴有MET 外显子14跳跃突变和5例MET扩增。所有患者既往接受克唑替尼,其中的3例患者也接受其他MET抑制剂。克唑替尼和capmatinib中位治疗间隙为22天(范围: 4–374天)。
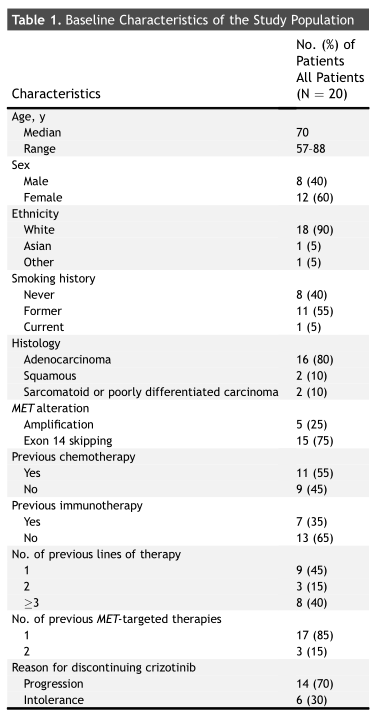
临床特征
研究数据表明, 2例患者 (10%) 达到了部分缓解 (PR)。在克唑替尼和capmatinib 治疗期间,都接受化疗联合pembrolizumab 。14例患者达到疾病稳定(SD),总的疾病控制率(DCR)为80%。其中两例SD患者几乎达到了PR(RECIST -28% and -25%)。很多患者取得了长达6个月的疾病稳定。MET 外显子14跳跃突变患者的ORR为13% (n =2/15),而MET扩增的患者ORR为0%(n=0/5)。4例伴有可测量脑转移瘤患者颅内控制率为100%,但是没有颅内临床缓解。
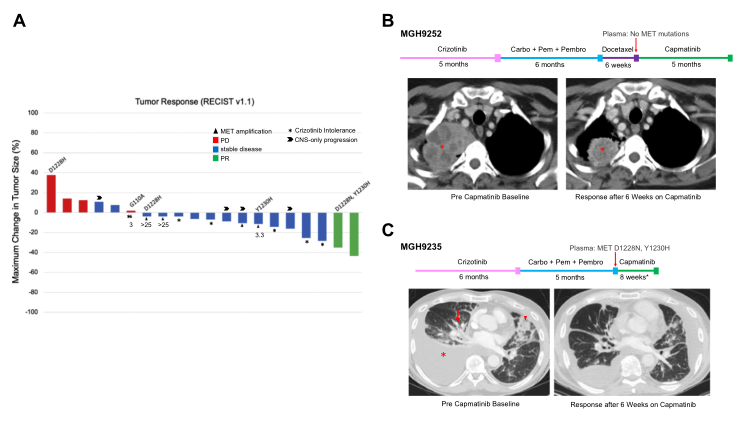
临床疗效
临床疗效
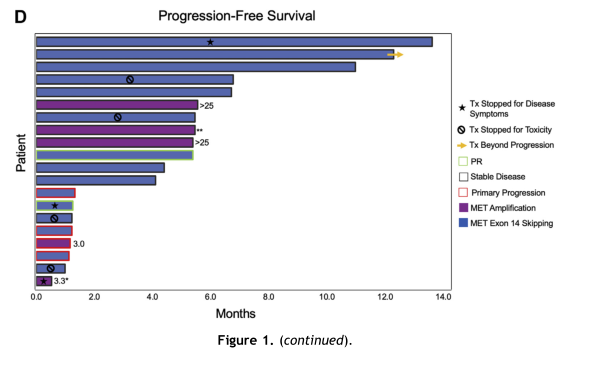
生存分析发现,中位PFS为5.5个月(95%CI: 1.3–11.0),OS为11.3个月(95%CI: 5.5–未达到)。
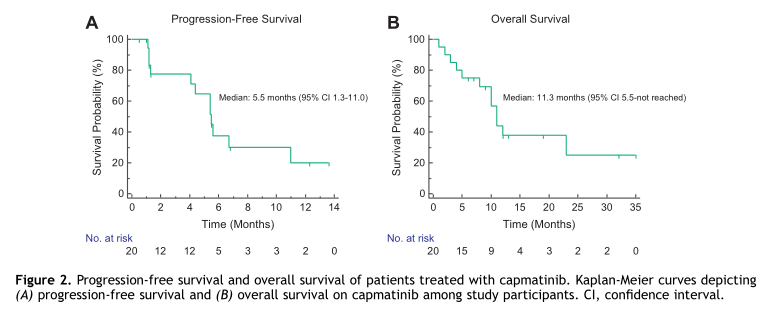
生存分析
不良事件分析,至少15%的患者中发生任何级别治疗相关不良事件,包括下肢水肿(n=13, 65%),疲劳(n=7, 35%),恶心(n=7, 35%),肌痛(n=4, 20%)、淀粉酶升高(n=4, 20%)、肌酐升高(n=4, 20%),脂肪酶升高(n=4, 20%),丙氨酸转氨酶升高(n=3, 15%)神经病变(n=3, 15%)。8例患者(40%)观察到3级治疗相关不良事件,包括无症状脂肪酶升高(n=3, 15%),淀粉酶升高(n=2, 10%),无症状天冬氨酸转氨酶(n = 1 , 5%)和丙氨酸转氨酶升高 (n = 1 , 5%)和呼吸困难(n=1, 5%)。未见有4级治疗相关不良事件发生。
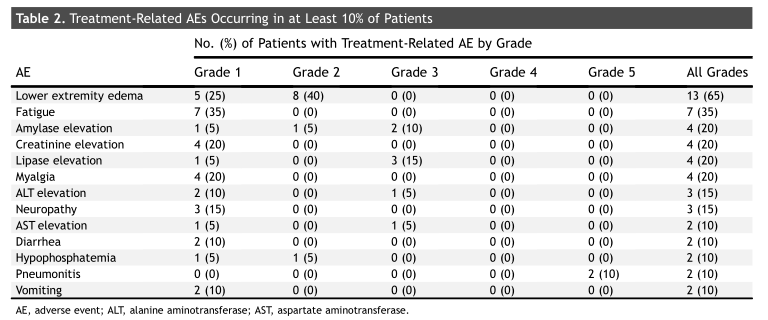
治疗相关不良事件
MET D1228 ,Y1230 突变和MAPK 改变在克唑替尼治疗后以及capmatinib治疗前的血浆中发现。Capmatinib治疗进展中的血浆检测可发现MET的持续以及新的突变,还有MARK基因改变。
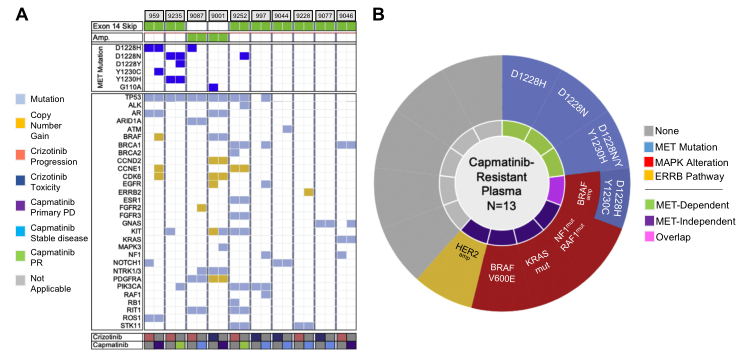
探索capmatinib耐药机制
综上,伴有MET基因改变的肺癌患者克唑替尼(crizotinib)治疗后再用Capmatinib治疗仍有中等疗效,可能归功于交叉的耐药机制。
原始出处:
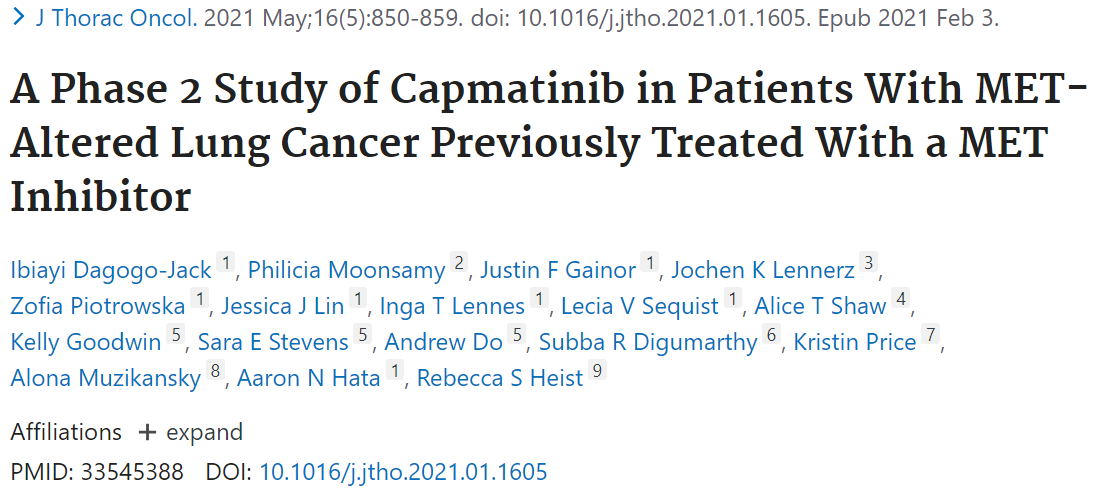
Ibiayi Dagogo-Jack, Philicia Moonsamy , Justin F Gainor,et al. A Phase 2 Study of Capmatinib in Patients With MET-Altered Lung Cancer Previously Treated With a MET Inhibitor. J Thorac Oncol. 2021 May;16(5):850-859. doi: 10.1016/j.jtho.2021.01.1605.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MET抑制剂#
33
#CAP#
0
#I期临床试验#
51
#MET#
27
#抑制剂#
36
#II期临床试验#
35
#I期临床#
0
#THORAC#
33
#Oncol#
39
#II期临床#
35