APLAR痛风治疗临床实践指南VS2019年中国指南,9大项目对比,一文总结!
2022-01-06 风湿新前沿 MedSci原创
亚太抗风湿病联盟(APLAR)发布2021年痛风治疗临床实践指南。此指南与中国的指南又有什么异同呢?一起看看吧
亚太抗风湿病联盟(APLAR)发布2021年痛风治疗临床实践指南。本文就其中的22条治疗建议进行了罗列,同时与国内《中国高尿酸血症与痛风诊疗指南( 2019) 》中提到的相似问题进行对比,探讨国内外指南对于高尿酸血症或痛风治疗的异同点。

 一、指南总则
一、指南总则
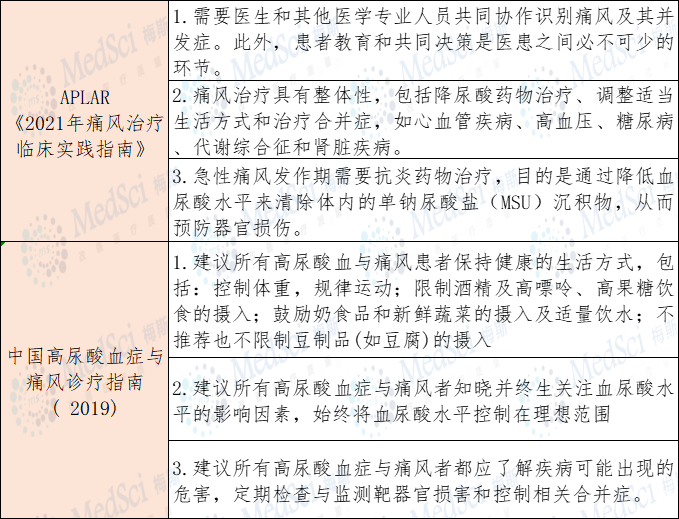
这两份指南对于高尿酸血症及痛风患者的总体指导原则总体相近,均提到了非药物治疗的重要性、关注相关并发症等方面的内容。

 二、无症状高尿酸血症的治疗
二、无症状高尿酸血症的治疗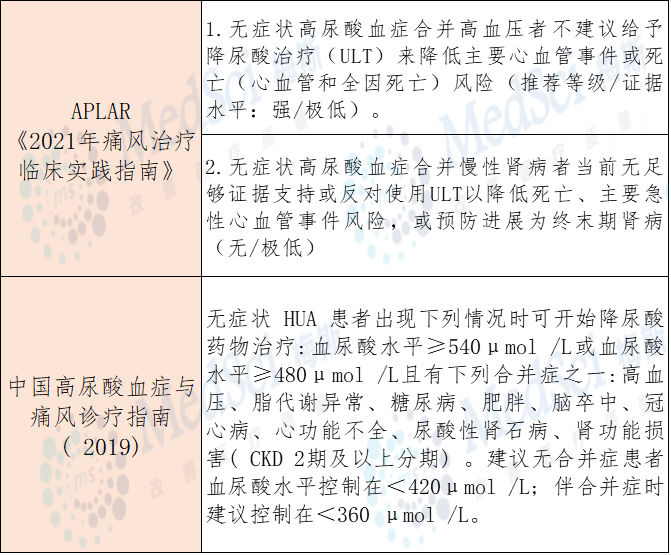
对于无症状高尿酸血症患者的药物治疗,各国指南观点不一,欧美指南多不推荐,而亚洲国家如日本、中国多持积极态度。

 三、急性痛风的治疗
三、急性痛风的治疗
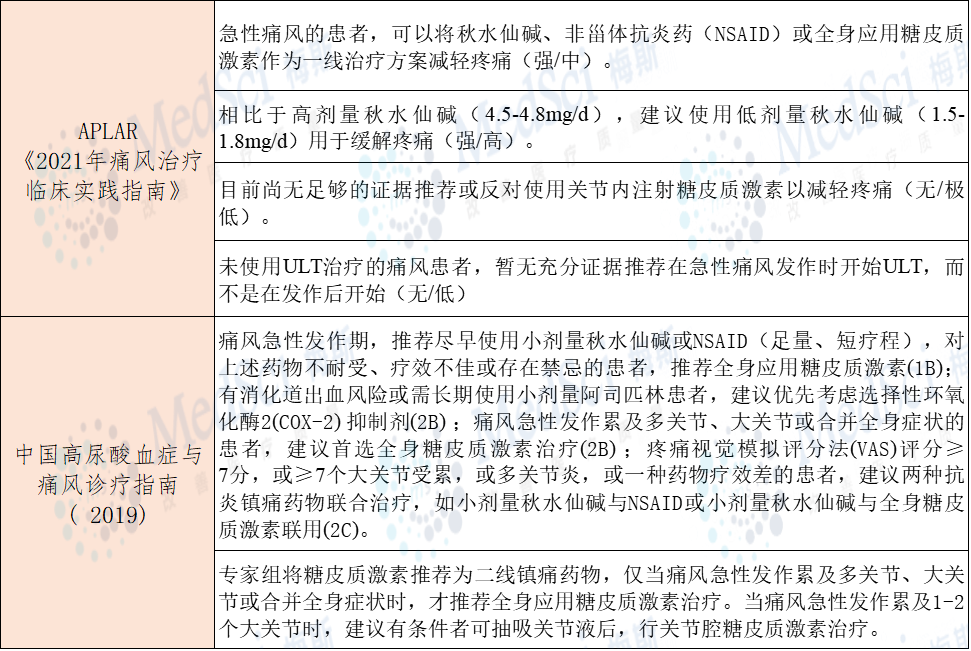
国内外学者均建议降尿酸治疗应在痛风急性发作完全缓解后开始,正在进行降尿酸治疗的急性发作患者不建议停药。两份指南均推荐将秋水仙碱、NSAID或全身应用糖皮质激素作为缓解疼痛的临床用药。

 四、开始降尿酸时痛风发作的预防
四、开始降尿酸时痛风发作的预防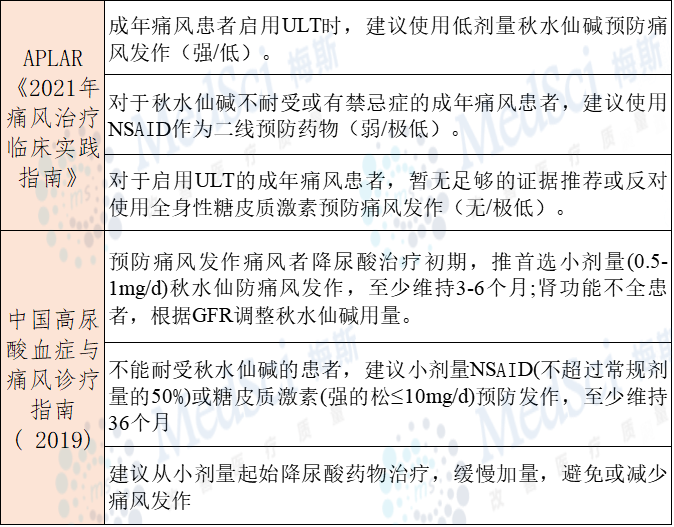
痛风急性发作的抗炎镇痛治疗两份指南意见基本相似。指南均推荐小剂量秋水仙碱预防痛风发作,无法耐受时可以选择NSAID或糖皮质激素治疗。

 五、降尿酸治疗
五、降尿酸治疗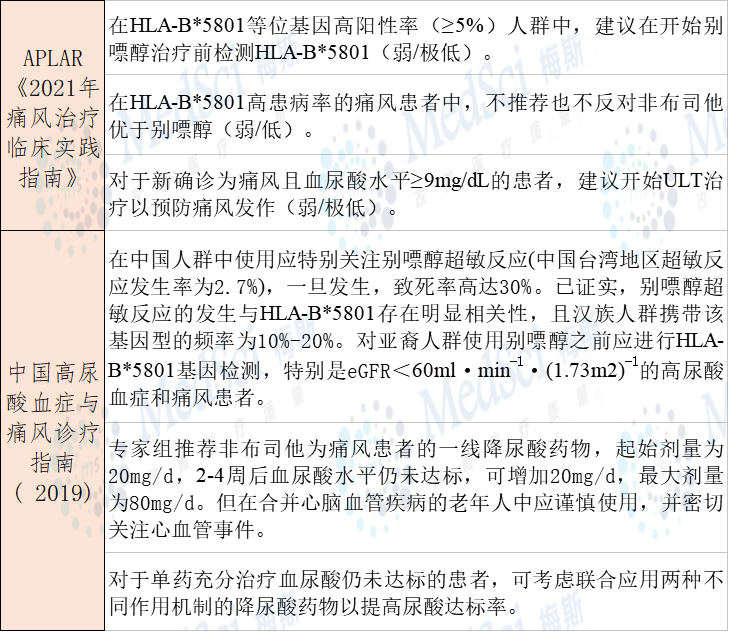
对于HLA-B*5801阳性患者,两份指南均不推荐使用别嘌醇。欧美指南多推荐非布司他为别嘌醇的替代用药,仅在别嘌醇不耐受或疗效不佳时使用。我国已将非布司他ULT的作为一线用药。

 六、慢性痛风石关节炎的治疗
六、慢性痛风石关节炎的治疗
对于慢性痛风石关节炎患者,建议使用黄嘌呤氧化酶抑制剂(别嘌醇或非布司他)溶解痛风石,而非无降尿酸治疗(强/低)。
在血尿酸水平>6mg/dL的慢性痛风石关节炎患者中,不建议在黄嘌呤氧化酶抑制剂治疗中添加新型降尿酸药物RDEA594(lesinurad),用于溶解痛风石(弱/中)。
《中国高尿酸血症与痛风诊疗指南( 2019)》中未提及慢性痛风石关节炎的治疗

 七、难治性和治疗无应答痛风的治疗
七、难治性和治疗无应答痛风的治疗
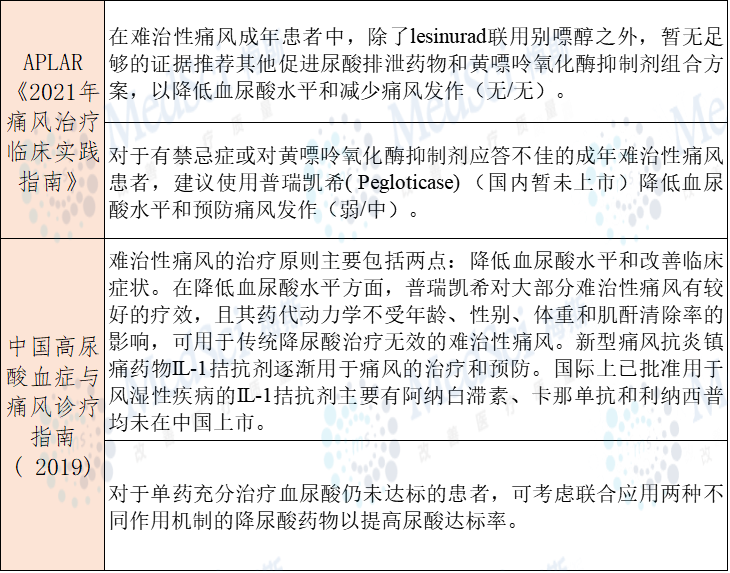
中国高尿酸血症与痛风诊疗指南( 2019)》中未提到lesinurad的使用,但在《痛风诊疗规范(2020)》中提到,lesinurad可用于单一足量使用黄嘌呤氧化酶抑制剂仍不能达标的痛风患者,可与黄嘌呤氧化酶抑制剂联合使用。对于可联用的黄嘌呤氧化酶抑制剂没有具体推荐。

 八、痛风合并中度至重度肾损害的治疗
八、痛风合并中度至重度肾损害的治疗慢性肾脏疾病是高尿酸血症与痛风患者常见合并症,为避免肾功能受损影响药物代谢和排泄,导致药物蓄积中毒,应根据肾功能分期合理选择降尿酸药物,及时调整药物的起始剂量和最大剂量。

 九、非药物治疗
九、非药物治疗
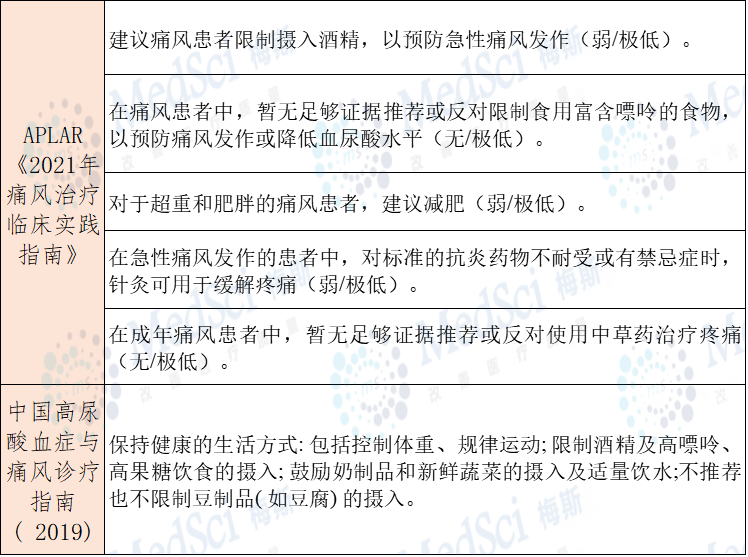
两份指南在高嘌呤饮食的意见不同。APLAR的最新指南并未提及豆制品,《中国高尿酸血症与痛风诊疗指南( 2019)》不推荐也不限制豆制品的摄入。
参考文献:
【1】.中国高尿酸血症与痛风诊疗指南(2019)[J]. 中华内分泌代谢杂志,2020,(01): 1-13.
【2】.Lorenzo JPP, Sollano MHMZ, Salido EO,et al. 2021 Asia-Pacific League of Associations for Rheumatology clinical practice guideline for treatment of gout[J]. Int J Rheum Dis. 2021 Dec 20.
【3】.徐东,朱小霞,曾学军,等. 痛风诊疗规范[J]. 中华内科杂志,2020(6).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#实践指南#
40
#中国指南#
47
#临床实践#
44
#APL#
48
#临床实践指南#
57
不错不错
55
实用
51