Nat Med: Dalpiciclib(达尔西利)或安慰剂+氟维司群治疗HR+/HER2-晚期乳腺癌的疗效和安全性对比:Ⅲ期DAWNA-1研究
2021-11-22 yd2015 MedSci原创
研究表明,DAWNA-1研究成果支持dalpiciclib(达尔西利)+氟维司群组作为既往治疗过的HR+/HER2-晚期乳腺癌的新选择。
2021年11月4日,Nature Medicine上发表了Ⅲ期DAWNA-1研究成果。该研究由中国医学科学院肿瘤医院徐兵河院士牵头,主要是评估国产原研的CDK4/6抑制剂dalpiciclib(达尔西利)治疗内分泌治疗耐药的HR+/HER2-晚期乳腺癌的疗效和安全性。
这是一项在全国39家医院进行的多中心、随机、对照、四盲(患者、治疗者、研究者、独立评审委员会)Ⅲ期临床研究。纳入内分泌治疗耐药的HR+/HER2-晚期乳腺癌,按2:1随机分配至Dalpiciclib(达尔西利)+氟维司群组(n=241)或安慰剂+氟维司群组(n=120)。主要研究终点为PFS(预设单侧P≤0.008为优效)。
在2019年6月25日至2020年9月2日期间,筛查了547名患者,361名符合条件的患者被随机分配到Dalpiciclib(达尔西利)+氟维司群组(n=241)或安慰剂+氟维司群组(n=120)。所有361例随机患者纳入疗效分析,360例治疗患者(dalpiciclib + 氟维司群组1例患者未接受治疗)纳入安全性分析。截至中期分析的数据截止日期(2020年11月15日),dalpiciclib + fulvestrant组241例患者中有144例(59.8%)仍在接受治疗,安慰剂+ 氟维司群组120例患者中有43例(35.8%)仍在接受治疗。中位随访时间分别为10.7个月(范围= 0.2 16.7)和10.6个月(范围= 0.8 16.7)。dalpiciclib +氟维司群组65例(27.0%)和安慰剂+氟维司群组49例(40.8%)在中断治疗后接受了至少1次后续抗肿瘤治疗。总体中位年龄为51.0岁;55.7%的患者是绝经后妇女,60.1%有内脏转移,72.6%曾接受过一次内分泌治疗。
在中期分析时,dalpiciclib联合氟维司群组241例患者中有86例(35.7%),安慰剂联合氟维司群组120例患者中有76例(63.3%)出现疾病进展或死亡。研究人员评估的dalpiciclib+氟维司群组和安慰剂组的中位PFS分别为15.7个月(95%CI:11.1~NR)和7.2个月(5.6~9.2个月);Dalpiciclib组的进展或死亡风险降低58%(HR 0.42,95%CI:0.31~0.58,单边P<0.0001)。Dalpiciclib +氟维司群组和安慰剂组+氟维司群组6个月和12个月的PFS率分别为76.4% (95% CI = 70.1 - 81.5) vs 53.2% (95% CI = 43.5 - 62.0)和51.8% (95% CI = 43.2 - 59.8) vs 29.1% (95% CI = 20.2 - 38.5)。独立评审委员会评估的dalpiciclib组和安慰剂组的中位PFS分别为13.6个月(95%CI:11.3~NR)和7.7个月(5.6~10.9个月);dalpiciclib组的进展或死亡风险降低55%(HR 0.45,95%CI:0.32~0.64,单边P < 0.0001)。
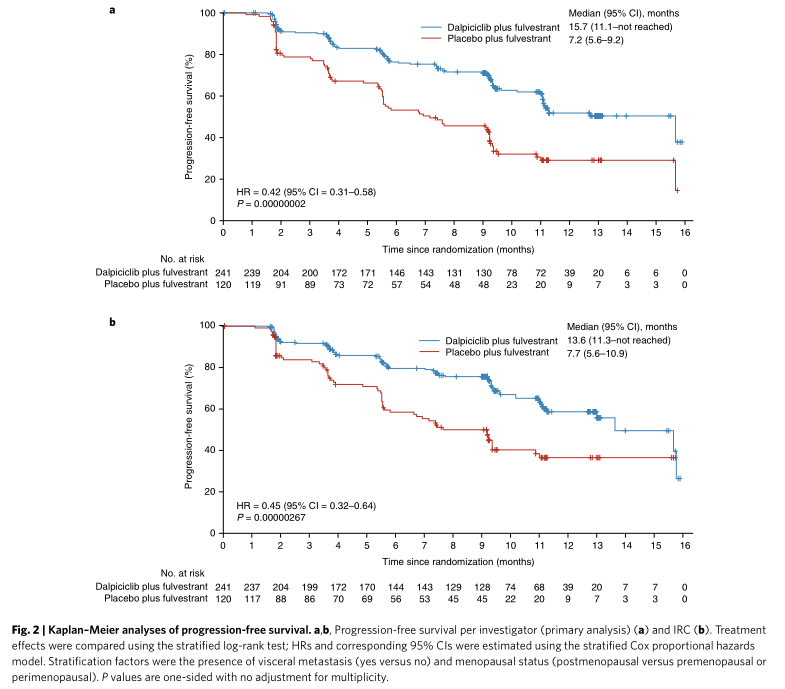
PFS
亚组分析发现,无论患者年龄、绝经状态、是否内脏转移、既往是否内分泌治疗及其线数、既往是否挽救化疗,dalpiciclib组与安慰剂组相比,PFS均有显著延长。
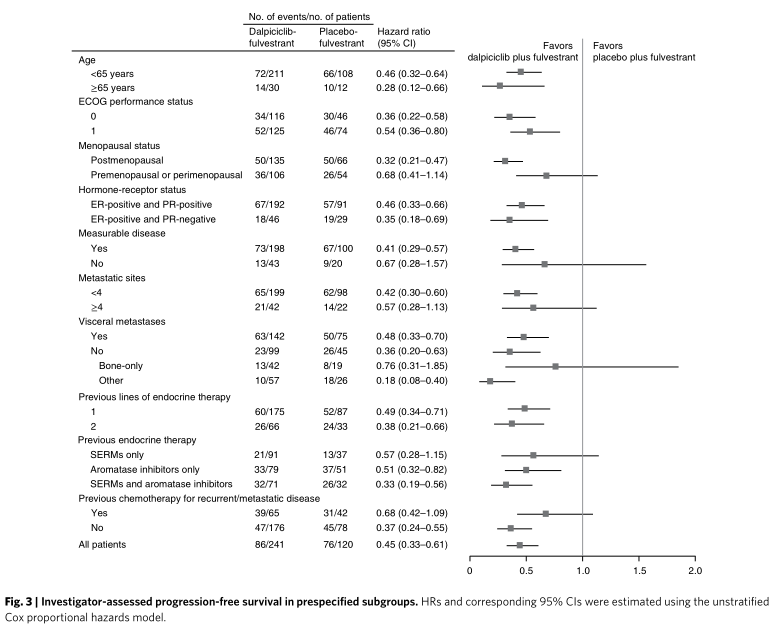
PFS亚组分析
在进行分析时,总生存数据尚不成熟,共记录了25例死亡: dalpiciclib +氟维司群组15例(6.2%),安慰剂组+氟维司群组10例(8.3%)。Dalpiciclib +氟维司群组58例(24.1%)患者和安慰剂+氟维司群组49例(40.8%)患者接受了后续化疗或死亡。Dalpiciclib +氟维司群组到第一次后续化疗或死亡的中位时间未达到,而安慰剂联合氟维司群组为14.2个月(95% CI = 9.-未达到)(HR = 0.47, 95% CI = 0.32 0.69; 单边P < 0.0001)。
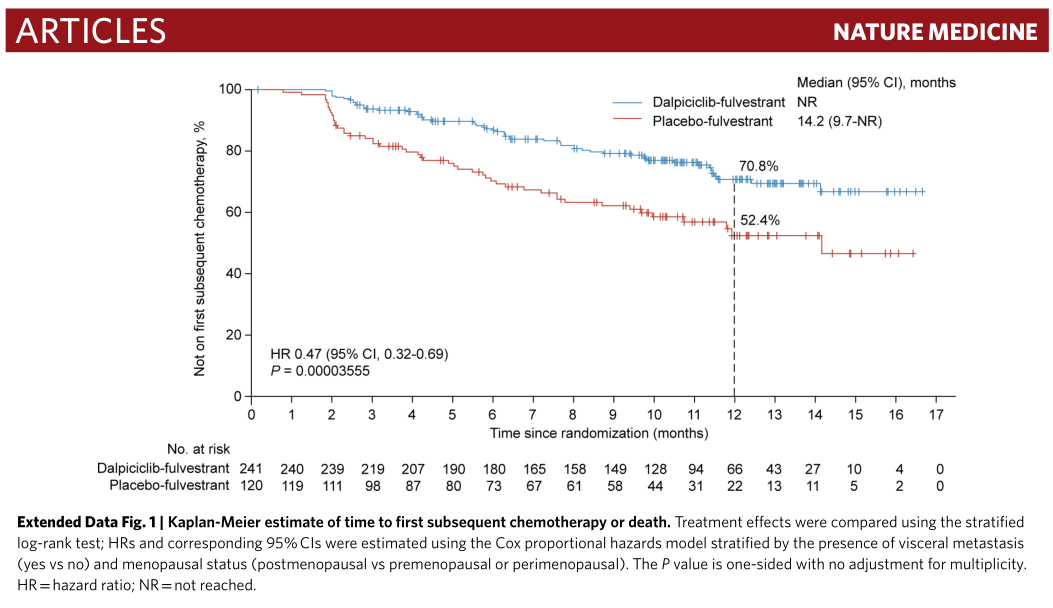
至第一次进展后化疗时间
根据研究人员的评估,dalpiciclib +氟维司群组与安慰剂组+氟维司群组的ORR分别为27.0% (95% CI = 21.5 - 33.0)和20.0% (95% CI = 13.3 - 28.3)。临床获益率分别为61.0% (95% CI = 54.5 - 67.2)和45.8% (95% CI = 36.7 - 55.2)。

疗效评估
Dalpiciclib +氟维司群组240例患者中有212例(88.3%)报告了3或4级不良事件(AEs),安慰剂组+氟维司群组120例患者中有16例(13.3%)报告了不良事件。分别有27.9%和1.7%的患者因为AEs导致剂量调整。Dalpiciclib组最常见的3级或4级AEs是中性粒细胞减少(84.2%)和白细胞减少(62.1%)。Dalpiciclib组和安慰剂组的严重AEs发生率分别为5.8%和6.7%。
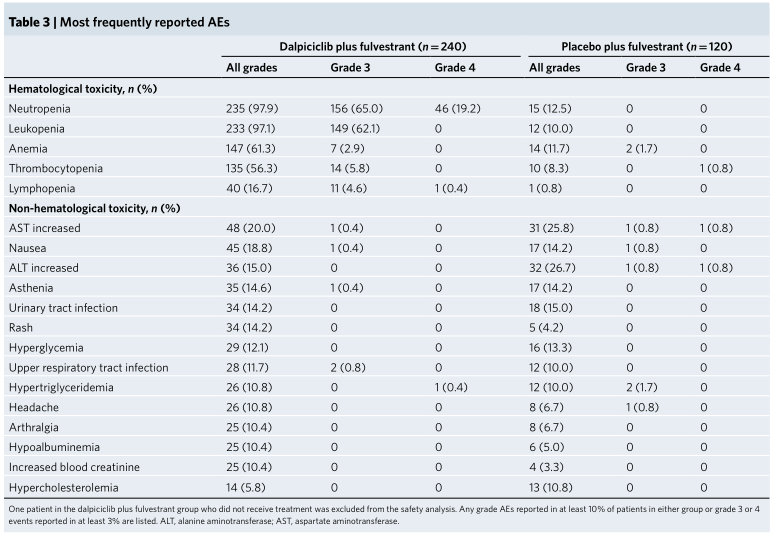
AEs
综上,研究表明,DAWNA-1研究成果支持dalpiciclib(达尔西利)+氟维司群组作为既往治疗过的HR+/HER2-晚期乳腺癌的新选择。
原始出处:
Xu B, Zhang Q, Zhang P, Hu X, Li W, Tong Z, Sun T, Teng Y, Wu X, Ouyang Q, Yan X, Cheng J, Liu Q, Feng J, Wang X, Yin Y, Shi Y, Pan Y, Wang Y, Xie W, Yan M, Liu Y, Yan P, Wu F, Zhu X, Zou J; DAWNA-1 Study Consortium. Dalpiciclib or placebo plus fulvestrant in hormone receptor-positive and HER2-negative advanced breast cancer: a randomized, phase 3 trial. Nat Med. 2021 Nov;27(11):1904-1909. doi: 10.1038/s41591-021-01562-9. Epub 2021 Nov 4. PMID: 34737452.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疗效和安全性#
51
#Nat#
40
#HER2-#
0
数据还是比阿贝差点意思, 人家都进医保咯
45
#ALP#
39
为国产达尔西利点赞
30
#安慰剂#
46
#Med#
31
中位随访时间分别为10.7个月(范围= 0.2
71