Clin Gastroenterology H: 胃经口内镜下幽门切开术治疗胃轻瘫的远期疗效分析
2021-03-29 MedSci原创 MedSci原创
胃轻瘫(GP)是一种慢性的,严重影响人生活质量的疾病,它以恶心,呕吐为早期为特征的疾病。每10万人的GP患病率男性是9.6,女性是37.8。
胃轻瘫(GP)是一种慢性的,严重影响人生活质量的疾病,它以恶心,呕吐为早期为特征的疾病。每10万人的GP患病率男性是9.6,女性是37.8。目前尚无明确的GP治疗方法,最有效的针对症状的对症治疗。不幸的是,促胃动力药物的使用常常受到限制,因为它会有副作用,包括心律不齐等。腹腔镜幽门切开术显示出在缓解胃瘫症状中的良好效果,可以使近60%–90%的患者获得缓解,这种手术方式称为胃内镜下胃幽门切开术(GPOEM),GPOEM是胃轻瘫的一种有前途的治疗方法,但是关于该手术的长期结果的数据很少。本项研究旨在探究GPOEM治疗难治性胃轻瘫患者的长期结果。
研究人员对2015年6月至2019年3月间97名接受GPOEM进行难治性胃轻瘫的患者进行了回顾性病例系列研究,其中90例患者有3个月以上的随访数据。胃轻瘫基本症状指数(GCSI)评分(餐后饱胀或早饱,恶心,呕吐和腹胀的测量)和SF-36问卷得分(测量生活质量)用来评估胃瘫程度。主要观察结局是对GPOEM的临床反应,定义为GCSI评分降低至少1分,而至少2个主要症状亚量表降低25%以上。复发的定义是,在初始完全缓解后至少2个月内,基线GCSI或GCSI评分恢复到3或更高。
在初次随访时(GPOEM后3到6个月),有73例患者(81.1%)在手术后获得临床反应,SF-36问卷评分显着增加(表明生活质量提高),而17例患者(18.9%)无反应。GPOEM六个月后,有7.1%的患者出现疾病复发。在12个月时,仍有8.3%的患者复发。在24个月时,研究中仍有4.8%的患者复发。在36个月时,有14.3%的患者出现胃瘫的复发。对于经历初始临床反应的患者,每年这种反应的丧失率为12.9%。在单变量和多变量回归分析中,胃轻瘫的持续时间越长,对GPOEM应答的几率就越小(几率[OR]为0.092; 95%CI为1.04–1.3; P = 0.001)。
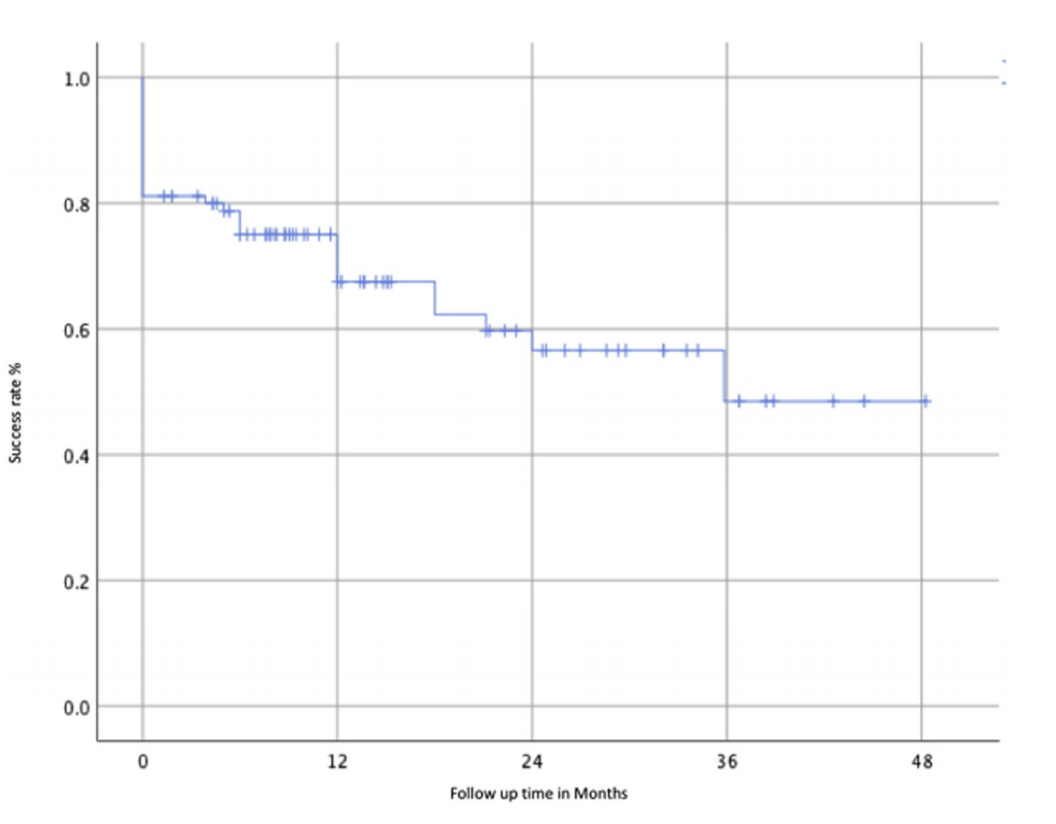
本项研究最后作者说道GPOEM治疗1年后,所有患者中有69.1%发生了临床反应,而85.2%的初始反应者保持了临床反应。手术后长达3年,患者一直保持临床反应并改善了生活质量,同时,作者发现高BMI和持续性胃轻瘫与GPOEM失败有关。
原始出处:
Mohamed M. Abdelfatah. Et al. Long-term Outcome of Gastric Per-Oral Endoscopic Pyloromyotomy in Treatment of Gastroparesis. Clinical Gastroenterology and Hepatology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#GAS#
27
#远期疗效#
40
#Gastroenterol#
39
#AST#
35
#疗效分析#
39
#内镜#
33
#Gastroenterology#
25
与贲门失弛缓思路差不多
80
谢谢梅斯提供这么好的信息,学到很多
50