双能计算机断层扫描测量肺血容量有助于区分肺动脉高压患者
2022-07-24 刘少飞 MedSci原创
在这项研究中,我们评估了 DECTPA 参数与超声心动图衍生的 SPAP 的相关性,并使用新的基于患者的图像采集协议将这些参数的预测能力与 PH 和右心应变的常规 CTPA 征象进行了比较。
肺动脉高压 (PH) 是一种复杂的危及生命的疾病,影响约 1% 的人口,老年人和左心衰竭患者的患病率增加。由于其非特异性临床症状,诊断可能会延迟到疾病晚期。虽然右心导管术 (RHC) 是确认诊断的金标准技术,但通常主要通过多普勒超声心动图或 CT 扫描等侵入性较小的方式提出。非侵入性方式也可能有助于减少这些患者治疗后随访中对重复 RHC 的需求。计算机断层扫描肺血管造影 (CTPA) 是疑似 PH 患者诊断检查的关键部分,可提供有关胸部结构和肺血管系统的详细形态学信息。双能量系统允许在不同千伏电压下进行同步图像采集。基于三材料分解算法,这些扫描有助于材料区分。在胸部影像学中,以碘图表示的整个肺实质中的碘分布测量已被用作肺血容量的估计值。该技术能够将功能信息添加到传统单一能量系统产生的单纯形态细节中,并与其他灌注研究所描绘的相应肺灌注图显示出良好的相关性。最近,几项研究显示了 DECTPA 有希望的实际益处,即改善急性肺血栓栓塞 (PTE) 的预后和提高慢性血栓栓塞性肺动脉高压 (CTEPH) 的诊断准确性。绝对肺动脉压 (PAP) 值与 DECTPA 参数之间的相关性一直是最近一些具有争议结果的研究的焦点。在这项研究中,我们评估了 DECTPA 参数与超声心动图衍生的 SPAP 的相关性,并使用新的基于患者的图像采集协议将这些参数的预测能力与 PH 和右心应变的常规 CTPA 征象进行了比较。
研究目的:
评估通过双能量计算机断层扫描肺血管造影(DECTPA)获得的全肺增强(WLE)和肺血容量(PBV)与超声心动图得出的收缩期肺动脉压力(SPAP)之间的相关性。
研究方法:
68名接受DECTPA检查的患者在获得知情同意后被纳入研究。在DECTPA研究的48小时内,对所有受试者进行了经胸超声心动图,以测量SPAP。评估了DECTPA衍生的两个参数,即WLE和PBV与SPAP的关联性。此外,这些参数的预测强度与传统的计算机断层扫描(CT)的肺动脉高压(PH)迹象进行了比较。
图 1. 显示研究人群和方法的研究流程图,以及 SPAP <30 和 SPAP >30 组的研究结果。
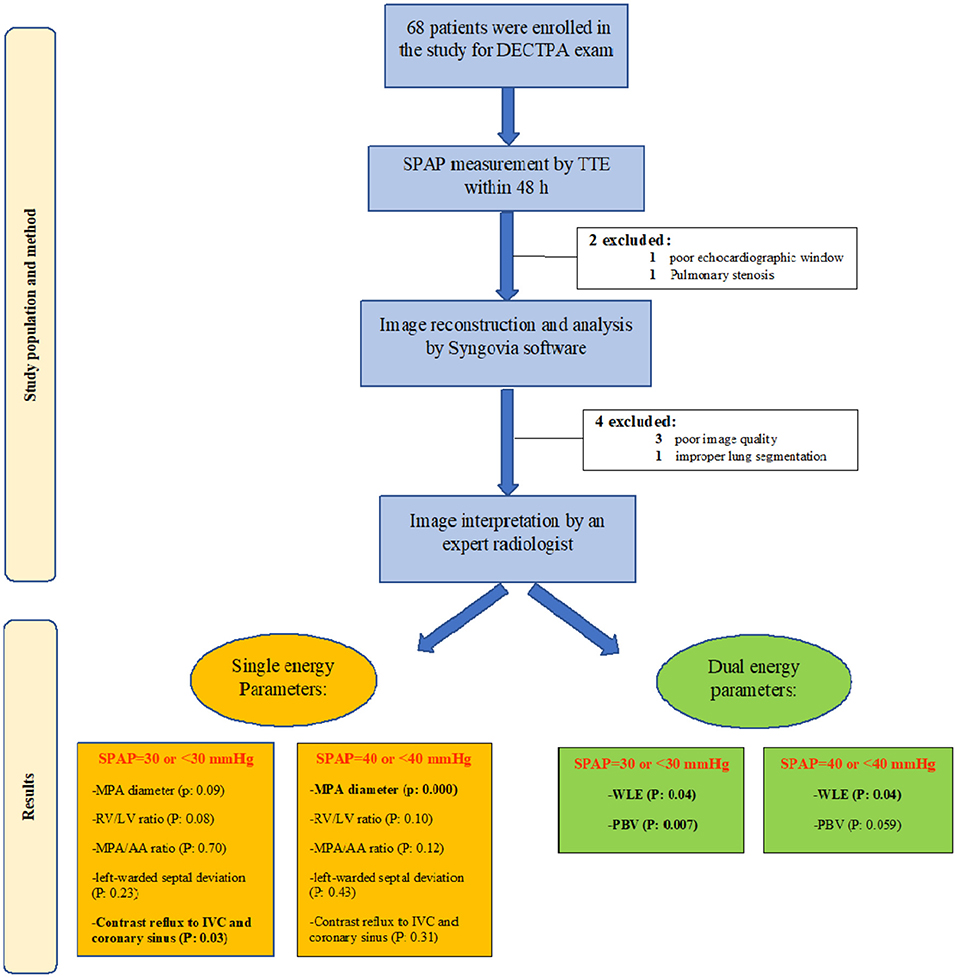
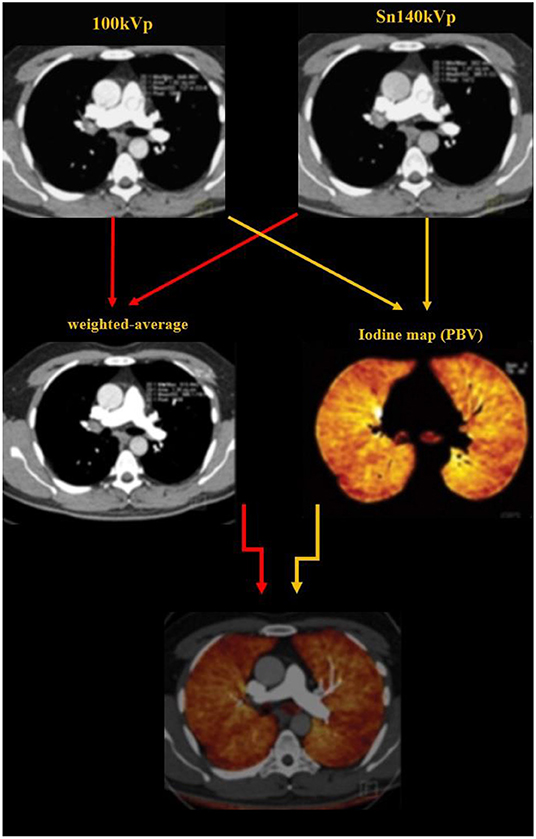
图 2. 图像重建作为三组图像进行:140 kV 图像、100 kV 图像和加权平均图像(分别来自 Sn 100 kVp 和 Sn 140 kVp 图像系列的 60% 和 40% 权重)。
研究结果:
SPAP值与主肺动脉(MPA)直径呈中度相关(r = 0.48,P < 0.001),而与WLE(r = -0.33,P = 0.007)、PBV(r = -0.31,P = 0.01)和MPA/升主动脉(MPA/AA)比率(r = 0.26,P = 0.03)呈弱相关关系。在回归分析中,MPA直径(B±SE:1.8±0.6,P=0.004)和WLE(B±SE:-0.5±0.3,P=0.042)与SPAP有明显关系。此外,SPAP≥30mmHg与右心室与左心室直径(RV/LV)之比[OR(CI 95%):24.39(1.3-573.2),P=0.04]有关,与PBV[OR(CI 95%):0.96(0.93-0.98),P=0.005]呈反向关系。获得的PBV截止值为83%,显示识别SPAP≥30mmHg的敏感性和特异性为73%[AUC(CI 95%):0.727(0.588-0.866),P=0.008]。
研究结论:
通过DECTPA对碘分布分析的自动后处理计算可以被认为是调查PH的辅助工具。
参考文献:
Rezaei-Kalantari K, Samimi K, Zomorodian H, Bakhshandeh H, Jafari M, Farahmand AM, Pourseyedian T, Sharifian M, Qanadli SD. Pulmonary Blood Volume Measured by Dual-Energy Computed Tomography Can Help Distinguish Patients With Pulmonary Hypertension. Front Cardiovasc Med. 2022 Jul 5;9:835655. doi: 10.3389/fcvm.2022.835655. PMID: 35865383; PMCID: PMC9294319.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血容量#
70
#计算机#
43
#动脉高压#
39
#肺动脉高压患者#
53
#期刊论坛##学习#
58