NEJM:万古霉素诱导的线性IgA大疱性皮肤病-病例报道
2020-10-15 MedSci原创 MedSci原创
该患者疑似为由万古霉素诱导的线性IgA大疱性皮肤病,并且终止了万古霉素治疗,同时继续使用头孢吡肟。该患者停用万古霉素治疗后1天,病变没有进一步发展。
患者为一名67岁的男子,因弥漫性皮疹1天而到急诊就诊。他有接受过放射疗法治疗的前列腺癌病史,并因尿道狭窄的发展而变得复杂,为此他接受了手术治疗。最近他又诊断有多发性耻骨骨髓炎和肌炎,开始用头孢吡肟和万古霉素治疗。抗生素治疗开始十天后,他注意到舌头有灼热感,随后红斑迅速发展,腹部、手臂和腿部出现水泡。
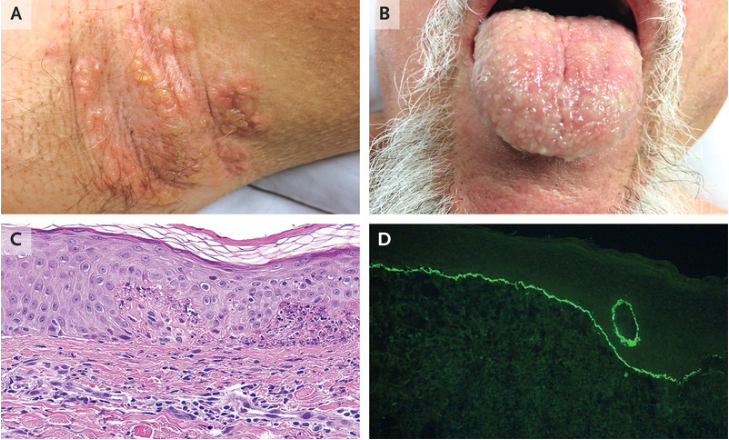
体格检查发现腋窝(如图A所示)和舌头(如图B所示)上有囊泡,腹部、手臂和腿上有囊泡的红斑,无发烧、嗜酸性粒细胞增多或器官功能障碍。活检标本的组织病理学检查发现有嗜中性乳头炎伴微泡(如图C所示,HE染色)。直接免疫荧光显示,IgA沿基底膜区线性沉积(如图D所示)。
该患者疑似为由万古霉素诱导的线性IgA大疱性皮肤病,并且终止了万古霉素治疗,同时继续使用头孢吡肟。该患者停用万古霉素治疗后1天,病变没有进一步发展。
在随访1个月时,该患者的粘膜皮肤病变完全消失。
原始出处:
J. Raymond Go,et al.Vancomycin-Induced Linear IgA Bullous Dermatosis.N Engl J Med 2020;https://www.nejm.org/doi/full/10.1056/NEJMicm2003334
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#皮肤病#
0
学习了
72
#IgA#
50
涨知识
0
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
54