贝伐珠单抗治疗肺癌脑转移伴难治性瘤周水肿的疗效
2021-11-20 MedSci原创 MedSci原创
肺癌患者中脑转移是常见的死亡原因,发生率较高,自然 病程低于 3 个月。除肿瘤细胞本身的倾斜性生长和不断增 殖,研究发现,90% 的脑转移会引发瘤周水肿,加重颅内压增高症状。该症状属于晚期急危肿瘤,在
肺癌患者中脑转移是常见的死亡原因,发生率较高,自然 病程低于 3 个月。除肿瘤细胞本身的倾斜性生长和不断增 殖,研究发现,90% 的脑转移会引发瘤周水肿,加重颅内压增高症状。该症状属于晚期急危肿瘤,在短时间内会继发脑疝,出现呼吸、心跳骤停等情况,导致患者死亡。因此,需在第一时间给予紧急处理,快速缓解临床症状。
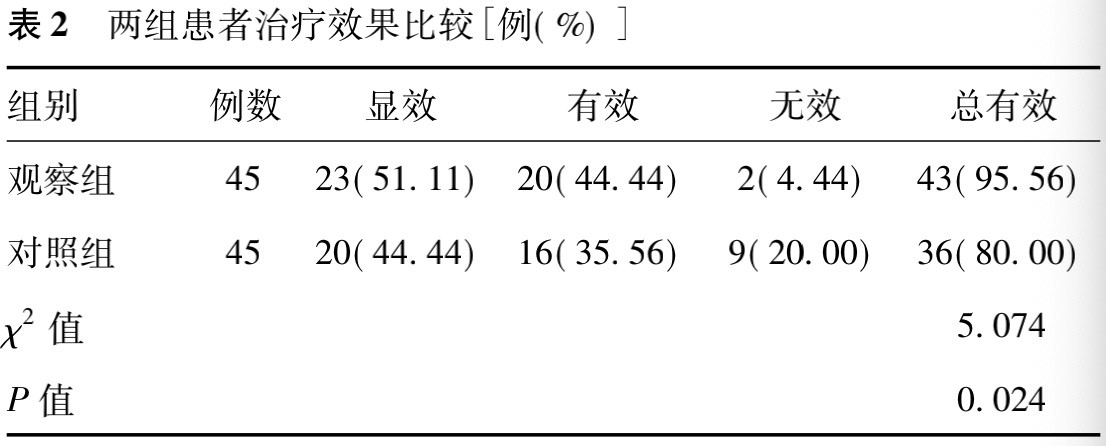
选择 90 例 肺癌脑转移的伴难治性瘤周水肿患者,采用计算机随机法将其分为两组,每组各 45 例。观察组与对照组分别给予贝伐珠单抗治疗与常规治疗,对比两组患者治疗前后生活质量评分,治疗总有效率及不良反应情况。
方法: ①对照组采取常规治疗,给予地塞米松,初始药物 剂量 0. 75 ~ 3 mg,4 次/d,之后 1 片/d,药物剂量为0. 75 mg,依 据患者实际病情进行有效调整,并给予静脉滴注甘露醇。与 此同时,患者接受放疗与化疗。②观察组给予贝伐珠单抗治 疗; 贝伐珠单抗的药物剂量为 5 mg /kg,用药间隔时间为 2 ~ 3 周。对于贝伐珠单抗联合全身化疗患者,应每间隔 3 周,进行 1 次给药。与放疗患者联合,需在放疗前给予 1 次用药,为减 轻放射性脑损伤及单纯减轻脑水肿,用药间隔 2 ~ 3 周,需依 据患者实际病情,决定用药情况。
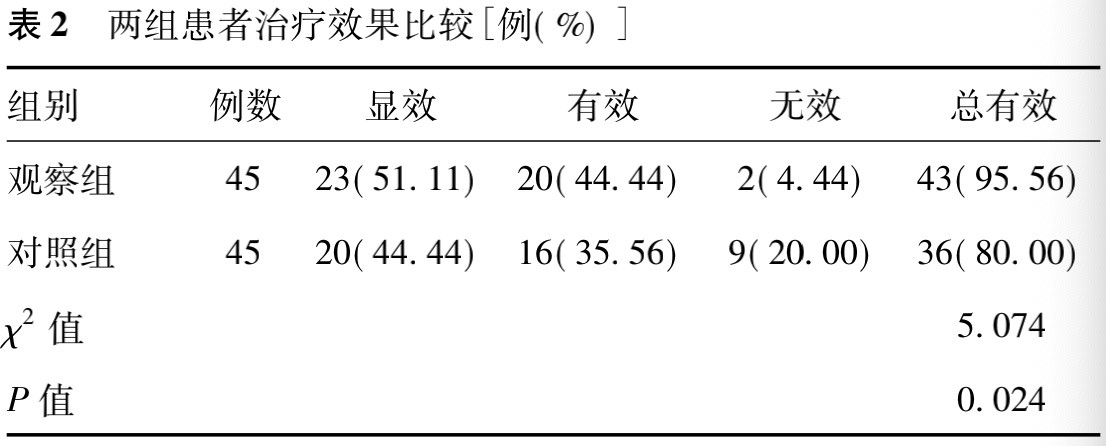
结合表中数据综上所述:两组患者治疗效果比较: 观察组治疗总有效率和对照组
比较,组间差异有统计学意义( P<0. 05) 。无论是单一用药,还是联合用药,贝伐珠单抗均能对瘤周水肿加以控制,与普通放化疗比较,该药物的起效时间更短。对于放疗或肿瘤引发的重度瘤周水肿,采取贝伐珠单抗具有良好 的治疗效果,但在后期随访中发现,与联合放化疗比较,单药单次使用贝伐珠单抗维持的治疗效果较短,而联合治疗可维持到 3 个月以上。分析原因,与放化疗联合,贝伐珠单抗可通过减少生成新生血管、改善细胞乏氧状态,促进血管壁结构正常,可提升放化疗的药物敏感作用,可见贝伐珠单抗具有提高放化疗效果的作用。
原始出处:
吉林医学 2021 年 2 月第 42 卷第 2 期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#贝伐珠#
45
#水肿#
43
#贝伐#
44
#难治性#
39