Nature: 首次发现“肺-脑-轴”!肺部细菌直接调控大脑小胶质细胞炎症反应
2022-03-10 Hong Chaoli brainnews
目前与大脑相关的概念很热:肠脑轴、肝脑轴、骨脑轴。其实还有肺脑轴!脑与肺存在交互作用:诱发大脑自身免疫的T细胞会迁移到肺组织中发展成为具备致病的效应细胞并作为长期记忆细胞存活;吸烟和肺部感染大大增加多
中枢神经系统(CNS)的自身免疫过程不仅依赖于神经组织,还受到外周器官的影响。研究表明吸烟和肺部感染显著升高罹患多发性硬化可能性。且过往研究表明,能够引起CNS自身免疫反应的T细胞在进入CNS之前会迁入肺组织定居,发展成为致病效应细胞和长期记忆细胞。
肺存在共生的微生物群,且受到外周环境中刺激物的持续影响。肺微生物影响哮喘、特发性肺纤维化和肿瘤的病理过程。但对于肺微生物是否影响、如何影响CNS的自身免疫过程,我们尚不清楚。
2022年2月23日,德国哥廷根大学医学中心Alexander Flügel和Francesca Odoardi在Nature发表论文,证实机体中存在肺脑轴:肺微生物菌群可通过脂多糖调控大脑免疫反应。研究发现,利用新霉素将肺微生物群转变为富LPS细菌门,能够使小胶质细胞转变为I型干扰素通路基因表达状态,从而显著抑制促炎反应、缓解自身免疫症状。
为了探究肺微生物群的改变是否影响CNS自身免疫反应,研究人员首先对大鼠进行一周的气管内新霉素灌注,对支气管肺泡灌洗液(BALF)进行16S rRNA测序,结果表明新霉素引起了肺微生物群失调。
研究人员通过向大鼠尾静脉注射髓鞘碱性蛋白 (MBP) 特异性T细胞(T- MBP细胞)后6小鼠气管内注射MBP和CFA,建立肺实验性自身免疫性脑脊髓炎(肺 EAE,图1)的大鼠模型。有意思的是,在构建上述肺EAE模型之前气管内注射新霉素改变肺组织的微生物菌群多样性后能够阻断EAE的发生。
作为补充数据,研究人员还证实了气管内新霉素灌注没有引起肠道微生物失调,并且新霉素直接处理TMBP细胞没有影响TMBP细胞的增殖和EAE的临床评分、新霉素皮下注射(不接触微生物)没有降低EAE的临床评分。
为了进一步证实新霉素引起的肺部微生物菌群改变是否具有缓解EAE症状,将从其肺泡提取出来的微生物菌群移植到另一种EAE模型大鼠中能够明显改善其症状。
上述结果充分表明气管内新霉素灌注通过引起肺微生物群失调抑制肺EAE的发展。

图1:肺实验性自身免疫性脑脊髓炎模型
肺微生物群失调通过LPS调节CNS自身免疫
为了找到肺微生物群失调如何导致上述结果,研究人员分析了气管内新霉素灌注后肺微生物的构成,发现革兰氏阴性拟杆菌比例显著升高,其中主要包括产黑色素普雷沃菌。气管内灌注灭活的产黑色素普雷沃菌显著降低了EAE的临床评分。
通过微生物组学技术发现新霉素引起肺组织菌群数量增加最多的是革兰氏阴性拟杆菌,具体为普雷沃氏菌(Prevotellaceae), Muribaculaceae和 Rikenellaceae等种属细菌。向EAE模型大鼠气管中移植产黑色素普雷沃菌(P. melaninogenica)能够改善其疾病症状。
大多数脂多糖(LPS)是由细菌分泌的,可通过血脑屏障进入大脑中,调控小胶质细胞功能。抑制LPS产生后可加重EAE疾病症状,而气管内或鞘内直接注射产黑色素普雷沃菌来源的LPS能够明显改善EAE模型疾病症状。这些结果表明LPS可作为肺微生物调控大脑炎症的关键介质。
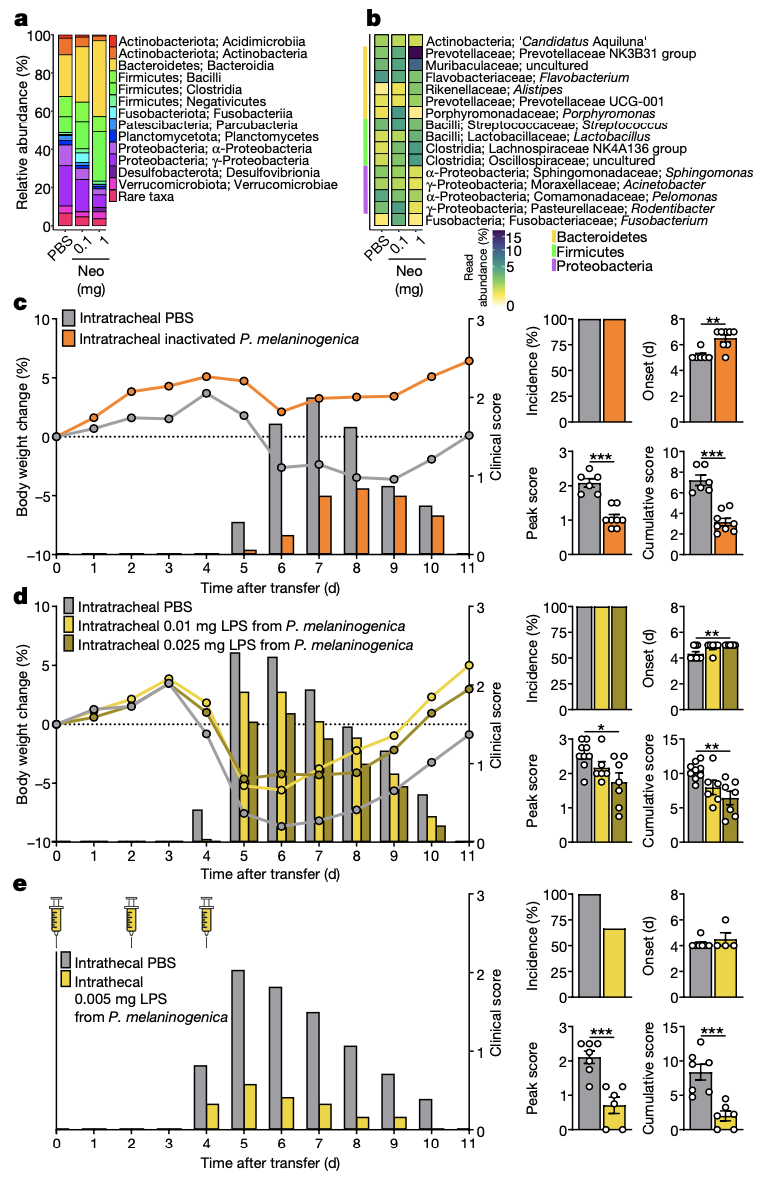
图2:肺LPS调节CNS自身免疫
肺微生物群失调影响小胶质细胞
CNS自身免疫反应依赖于迁入的TMBP细胞转变为II型干扰素通路基因表达状态、释放细胞因子、激活CNS中的免疫细胞和募集外周免疫细胞。研究结果显示气管内新霉素灌注显著降低了肺EAE模型大鼠的CNS中CD4+T细胞、CD8+T细胞、B细胞、巨噬细胞的数量,但不显著影响上述免疫细胞的基因表达。
研究人员猜想TMBP细胞通过影响小胶质细胞导致了上述结果。qPCR结果显示气管内新霉素灌注显著降低了小胶质细胞CXCL9、CXCL10、CXCL11、iNOS和 MHC-II的表达。利用米诺环素或CSF1R抑制剂抑制小胶质细胞显著降低了肺EAE的临床评分,且气管内新霉素灌注不会使米诺环素或CSF1R抑制剂更有效。
肺微生物群失调导致进入CNS的TMBP细胞数量显著降低
气管内新霉素灌注没有影响肺和血液中的TMBP细胞数量,也没有改变TMBP细胞的基因表达谱。活体双光子激光扫描显微术也显示新霉素没有改变TMBP向软脑膜血管中迁移的模式。血管内皮细胞的基因表达也不受影响。但气管内新霉素灌注显著降低了CNS中的TMBP细胞数量。
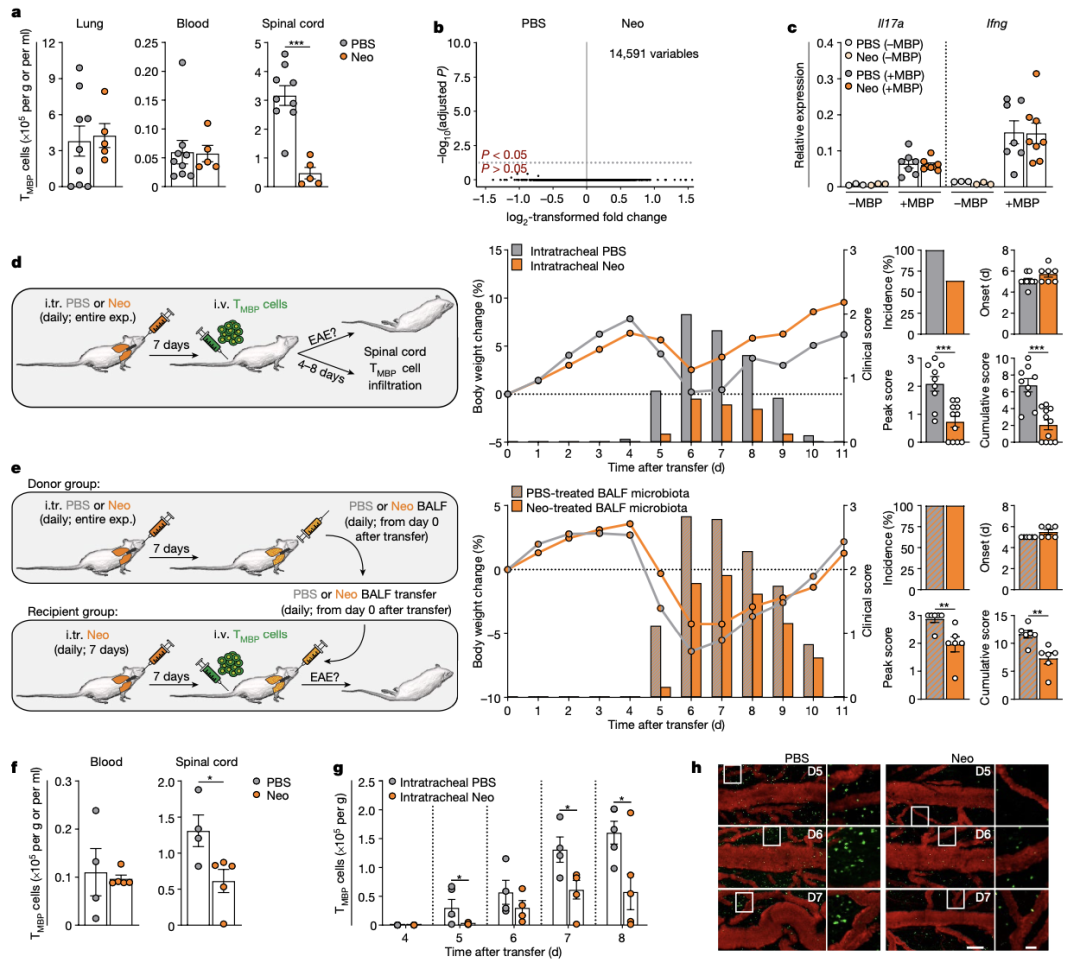
图3:肺微生物群失调不影响T细胞的激活和迁移
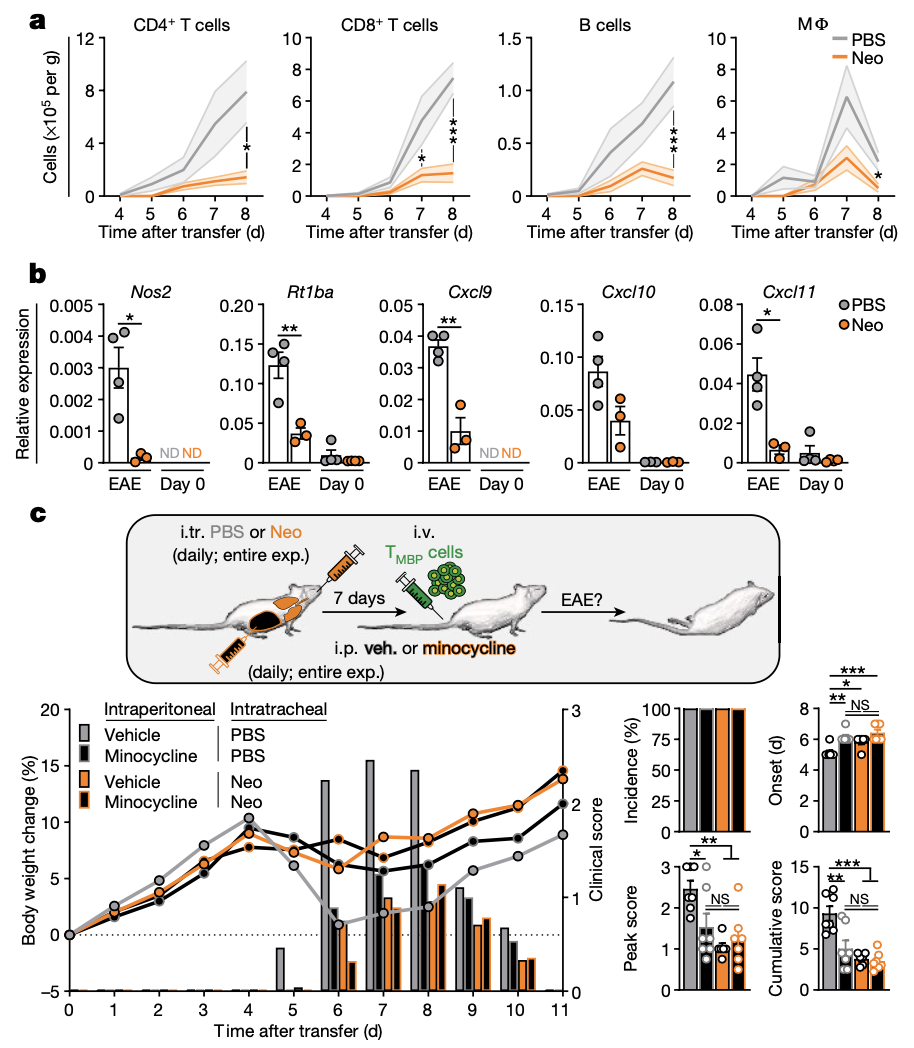
图4:肺微生物群失调影响小胶质细胞免疫反应
小胶质细胞的基因表达谱分析结果显示,I型干扰素信号通路基因的表达显著升高。鞘内注射poly I:C诱导小胶质细胞I型干扰素通路基因表达状态显著降低了肺EAE的临床评分。
以上结果说明,气管内新霉素灌注通过使小胶质细胞转变为I型干扰素通路基因表达状态,抑制CNS自身免疫反应。
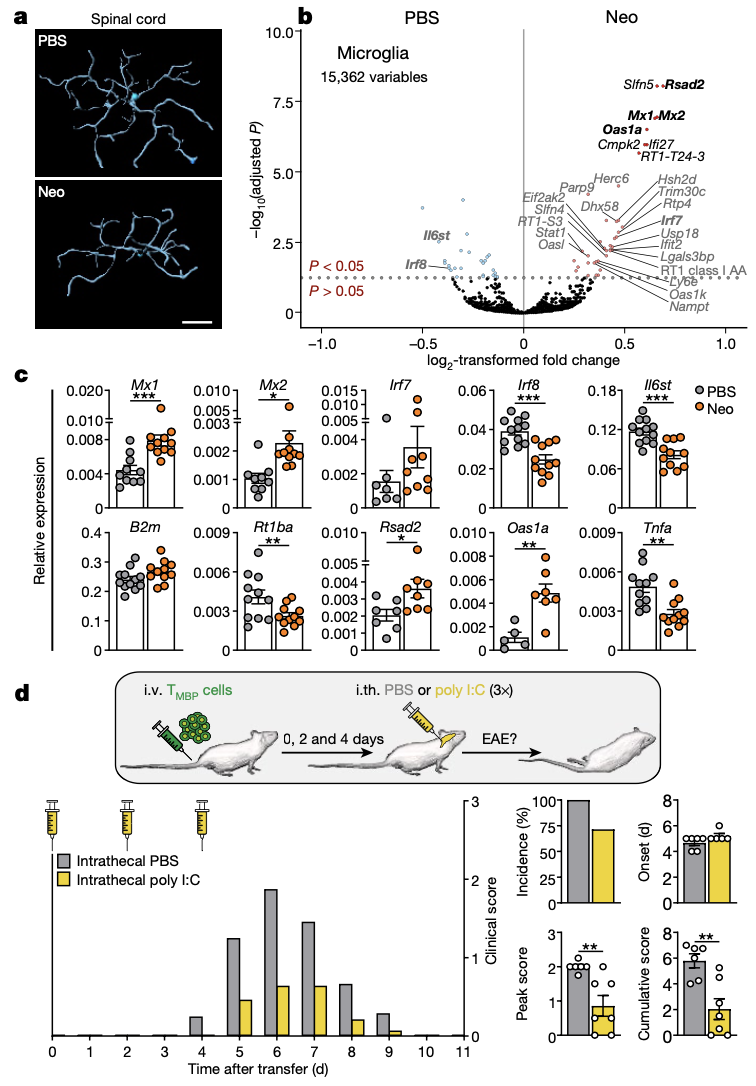
图5:肺微生物群失调使小胶质细胞转变为I型干扰素通路基因表达状态
总的来说,本文成功构建肺EAE模型,基于该模型揭示了肺微生物可直接作用于大脑免疫细胞-小胶质细胞,发挥免疫调控作用。将肺微生物菌群在中枢神经系统中的作用推向新的高度!
原文链接:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
30
#细胞炎症#
45
学习了
48
#炎症反应#
44
#胶质细胞#
56
学习一下
62