CHC 2014中国急性心梗注册研究(CAMI Registry)初步结果揭晓
2014-08-10 卢芳 CHC2014每日新闻
在中国心脏大会(CHC2014)上,阜外心血管病医院杨跃进教授报告了中国急性心肌梗死注册研究(CAMI Registry)的初步分析结果。 杨跃进 教授 杨跃进介绍,目前共有109 家医院参与CAMI 注册研究,每个省将有代表性地入选至少一家省级医院、一家地市级医院和一所县
在中国心脏大会(CHC2014)上,阜外心血管病医院杨跃进教授报告了中国急性心肌梗死注册研究(CAMI Registry)的初步分析结果。

杨跃进 教授
杨跃进介绍,目前共有109 家医院参与CAMI 注册研究,每个省将有代表性地入选至少一家省级医院、一家地市级医院和一所县医院。该研究截至到6 月底,已经入选患者超过2.3万例。本次在中国心脏大会报告的研究结果为截至到3 月底的结果,共分析16023 例患者。
其中73.5% 为ST 段抬高型心肌梗死患者(STEMI)。有42.6% 的STEMI 患者进行了急诊PCI 治疗,10.3% 进行了溶栓治疗。有8.8% 的非ST 段抬高型心肌梗死患者(NSTEMI)接受了急诊PCI 治疗。
在接受急诊再灌注治疗的STEMI 中,从到院到接受急诊再灌注治疗的时间存在很大的问题。到院到接受急诊PCI 治疗(D2B)的中位时间为165 分钟,从入院到溶栓时间(D2N)为130 分钟。满足指南D2B<90 分钟和D2N<30 分钟的患者比例24.3% 和19.6%。
该研究还分析了不同级别医院的治疗模式和院内预后情况。发现三个级别的医院的患者存在明显的差别:其中有到省级医院就诊的医院有36.1% 为转诊,而县医院仅有4.2% 为转诊。
到省级医院就诊的患者仅有17% 左右的患者能在发病3 小时内到达医院,县医院的患者则有30% 能在3 小时内到达医院。
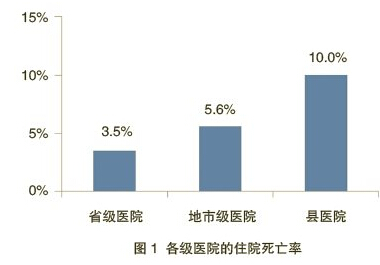
在校正相关危险因素后,省级医院的住院死亡率为3.5%,市级医院为5.6%,而县级医院为10%(图1)。
杨教授指出,中国急性心肌梗死普遍就诊较晚,其中,22.4% 和38.9%的STEMI 和NSTEMI 患者在发病后超过24 小时到达医院。中国的医院需要在心梗急性期尽早进行再灌注治疗。
CAMI还发现,当心肌梗死发作时,中国六成患者会表现为前胸部剧痛、大汗淋漓,其次是胸闷、心梗引起的身体其他部位的放射痛。还有极少数患者会表现为烦躁不安、黑曚或晕厥、持续上腹痛、牙或下颌疼痛以及大小便失禁。
研究还发现,男性和年轻患者常有明确的诱因。最常见的是体力应激、过度不良生活方式、精神应激、天气和环境骤变等。
在中国的心肌梗死患者中,54.4%的人目前吸烟或已戒烟,51.2% 的人患有高血压,53.9% 的人超重或肥胖。75% 以上的心梗患者缺乏运动、喜肥腻饮食。
九成患者至少伴有高血压、吸烟、糖尿病、超重或肥胖以及高血脂等心血管病危险因素中的一种,35% 的患者伴有3 种或3 种以上的危险因素。
相对老年患者,年轻患者中,男性、吸烟、高血脂、冠心病家族史更为多见。相对男性而言,女性患者更多合并高血压和糖尿病,更缺乏运动。
CAMI 研究是目前国内最大规模的急性心肌梗死注册研究,属十二五科技部支撑项目,由阜外心血管病医院牵头,共有全国109 家医院参加,分析了2013 年1 月1日~2014 年3 月31 日在发病7 天之内就诊的16023 例急性心肌梗死患者,平均年龄为61.8岁。其中74% 为男性,有19.5% 伴有糖尿病。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Registry#
37
#注册研究#
38
#CAM#
45
#急性心梗#
39
#GIST#
35
#CHC#
28
#注册#
25