Sci Transl Med:帕金森病的源头,竟然是你的阑尾?
2018-11-02 佚名 转化医学网
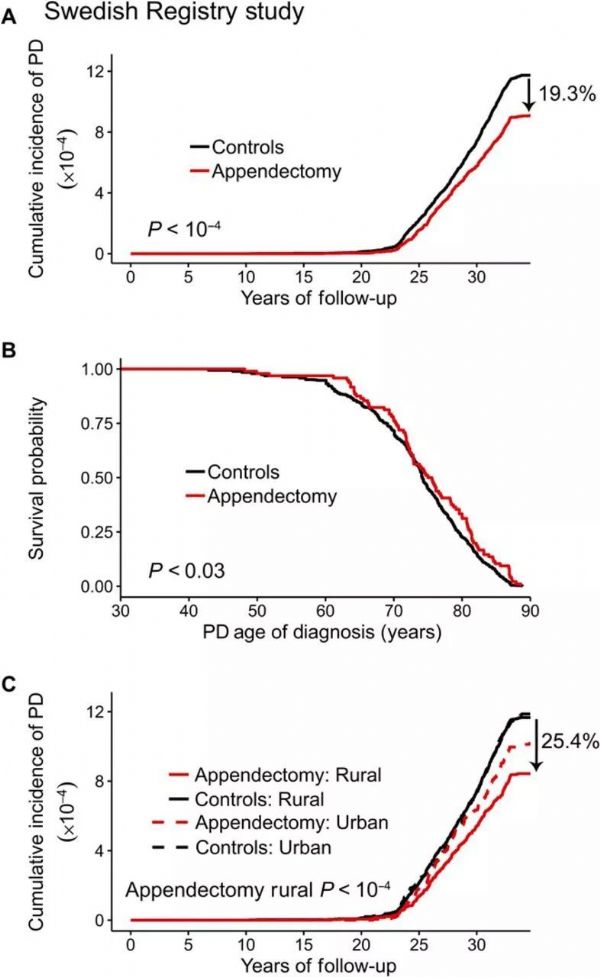
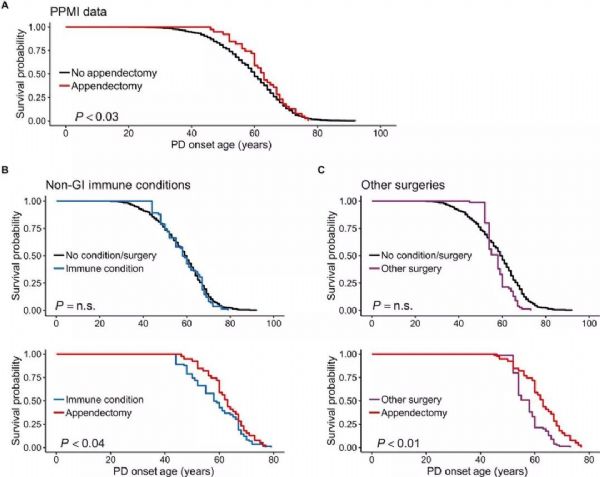
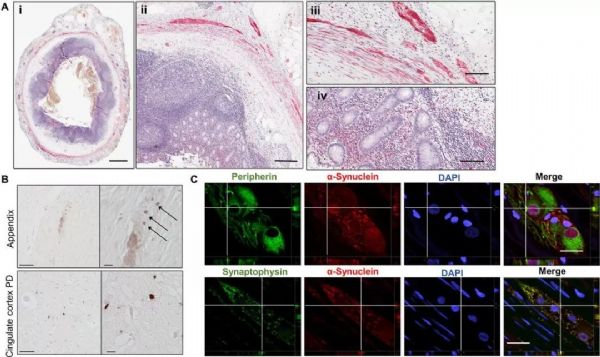
帕金森病最主要的病征是震颤,就如同图中阿里一样,除此以外,还会导致肌强直与运动迟缓,更为严重的是,约有 40% 的患者还出现了诸如抑郁症、痴呆的精神问题,严重者还会因并发症而死亡。然而帕金森病的具体发病原因究竟是什么,至今也仍不清楚,年龄老化,家族遗传,环境毒物等原因都可能导致帕金森病,而最新的一篇研究,将帕金森病与阑尾联系在了一起。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Transl#
35
#TRA#
38
#Med#
32
学习了谢谢分享
76
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
74