Int J Pediatr Otorhinolaryngol:生活方式相关的一些因素能够影响耳鼻喉疾病的患病率
2020-02-29 AlexYang MedSci原创
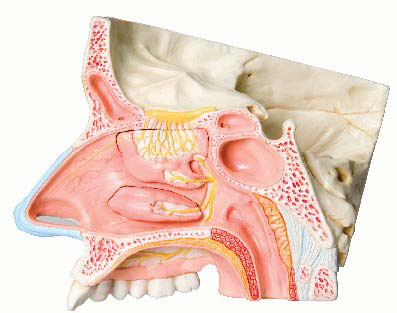
在最近几十年,研究人员注意到了久坐行为(SB)增加和身体活动(PA)减少的情况。最近,有研究人员确定了耳鼻喉疾病的发展与PA和SB之间的相关性。研究的数据来源于一个基于学校的关于小学、初中到高中儿童生活方式因素的调查研究。响应者会被提问SB、PA和耳鼻喉的情况:腺样体肥大(AH)、鼻窦炎(RS)和过敏性鼻炎(AR)。研究发现,清洁/吸尘的频率与AH的患病率有着显著的相关性。RS的患病率和工作日基于
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
27
#耳鼻喉#
31
#PE#
34
#患病率#
36
学习了,学习了
65
学习了,谢谢分享
70