【专家述评】| 腹膜转移癌腹腔化疗的创新与挑战
2024-10-24 中国癌症杂志 中国癌症杂志 发表于上海
本文通过梳理IPC研究的最新进展、不足和未来发展方向,以期为腹膜转移癌更有效的临床治疗提供可行性方向。
[摘要] 腹膜转移癌是指从原发部位扩散至腹膜的恶性肿瘤,常见于胃癌、结直肠癌、卵巢癌及腹膜假黏液瘤(pseudomyxoma peritonei,PMP)等多种癌症类型的晚期阶段。腹膜转移癌的复发率和死亡率高,严重危害人类健康,通常在根治术后或晚期腹膜转移阶段采用以化疗为主的姑息性治疗方案。腹膜转移癌治疗的难点在于缺少靶向治疗药物以及药物较难透过血-腹膜屏障,以致全身治疗效果欠佳。腹腔化疗(intraperitoneal chemotherapy,IPC)作为一种重要的临床治疗手段,在腹膜转移癌的治疗中具有广阔的应用前景。近年来,腹腔热灌注化疗(hyperthermic intraperitoneal chemotherapy,HIPEC)、腹腔加压气溶胶(pressurized intraperitoneal aerosol chemotherapy,PIPAC)等IPC技术的革新和新型药物的出现显著延长了患者的生存期。然而,腹膜转移癌的多样性和复杂性使临床IPC在给药方式、药物类型和剂量等治疗策略上仍然存在差异性和疗效不确定性。尽管已经制定了基于循证医学证据的指南和推荐治疗策略,但是仍需要通过更多的临床试验和更高级别的循证医学证据来进一步支持这些方案。本文对IPC的发展历程和最新进展进行归纳总结,对比分析手术治疗联合传统IPC、HIPEC及PIPAC等治疗手段的疗效,并对近期开展的IPC技术的研究进展进行汇总。此外,在IPC技术的临床应用方面,本文详细阐述其在胃癌、结直肠癌、妇科肿瘤、PMP、胆管癌及胰腺癌等疾病中的应用。针对IPC技术的局限性,提出纳米药物的创新开发有望为腹膜转移癌的治疗提供更安全有效的选择。综上所述,本文通过梳理IPC研究的最新进展、不足和未来发展方向,以期为腹膜转移癌更有效的临床治疗提供可行性方向。
[关键词] 腹膜转移癌;腹腔化疗;腹腔热灌注化疗;腹腔加压气溶胶;纳米药物;靶向治疗
[Abstract] Peritoneal metastatic carcinoma refers to the spread of malignant tumors from the primary site to the peritoneum. It is commonly observed in the advanced stages of various cancer types, including gastric cancer, colorectal cancer, ovarian cancer and pseudomyxoma peritonei (PMP). Peritoneal metastatic carcinoma seriously impair human health due to their high recurrence and mortality rates, and palliative treatment based on chemotherapy is usually provided after radical surgery or in the advanced stage of peritoneal metastases. The difficulties in the treatment of peritoneal metastatic carcinoma are the lack of targeted drugs and the difficulty of drugs to cross the blood-peritoneal barrier, resulting in poor systemic effects. Intraperitoneal chemotherapy, as an important therapeutic means, has a broad application prospect in the treatment of peritoneal metastatic carcinoma. In recent years, innovations in intraperitoneal chemotherapy techniques such as hyperthermic intraperitoneal chemotherapy (HIPEC), pressurized intraperitoneal aerosol chemotherapy (PIPAC) and the development of novel drugs have significantly improved patients' quality of life. The development of novel drugs has significantly improved patient survival. However, the diversity and complexity of these diseases have led to clinical variability and uncertainty in the efficacy of intraperitoneal chemotherapy in terms of treatment strategies such as mode of administration, drug type and dose. Although evidence-based guidelines and recommended treatment strategies have been developed, there is a need to further support these regimens through additional clinical trials and higher levels of evidence-based medicine. This review summarized the development history and recent advances in intraperitoneal chemotherapy, compared and analyzed the treatments such as surgery combined with traditional IPC, HIPEC and PIPAC, and summarized the research progress of recently conducted intraperitoneal chemotherapy techniques; moreover, in terms of the clinical application of intraperitoneal chemotherapy techniques, this paper elaborated on its use in diseases such as gastric cancer, colorectal cancer, gynecological oncology, PMP, cholangiocarcinoma and pancreatic cancer. For the limitations of intraperitoneal chemotherapy technology, it is proposed that the innovative development of nanomedicine is expected to provide a safer and more effective option for the treatment of peritoneal metastatic carcinoma. In conclusion, this review summarized the latest progress, shortcomings and future development of intraperitoneal chemotherapy, with the aim of providing a feasible direction for more effective clinical treatment of peritoneal metastatic carcinoma.
[Key words] Peritoneal metastatic carcinoma; Intraperitoneal chemotherapy; Hyperthermic intraperitoneal chemotherapy; Pressurized intraperitoneal aerosol chemotherapy; Nano-drug; Targeted therapy
1 引言
腹膜转移癌大部分为胃癌、结直肠癌、卵巢癌及腹膜假黏液瘤(pseudomyxoma peritonei,PMP)等的转移癌,一旦出现基本被认定为终末期肿瘤,治疗手段有限且患者预后不良[1-2]。多项研究及2022年版中国肿瘤整合诊治指南统计指出,20%的胃癌[3]、7%~15%的结直肠癌[4]、 75%的卵巢和95%的PMP[5]会发生腹膜转移。对于早期侵犯区域较小或转移病灶较局限的腹膜转移癌,通常采用以术后辅助化疗为主的综合治疗策略;而对于已出现弥漫性转移的腹膜转移癌患者,通常采用以化疗为主的姑息性治疗以减轻肿瘤负担、缓解症状[5]。化疗主要通过静脉注射或口服给药[6],但是血-腹膜屏障限制了药物由体循环进入腹膜腔,进而造成了常规化疗方式给药的疗效不佳[7-8],因此腹腔化疗(intraperitoneal chemotherapy,IPC)可作为一种更为理想的给药方式。
IPC能够直接将药物输注到腹膜腔中,是一条非传统的药物递送途径[9]。IPC通过提高药物在腹腔内的局部浓度[10],能够降低全身毒性[11],目前已成为腹膜转移癌治疗领域的研究热点。尽管IPC在治疗腹膜转移癌方面展现出巨大潜力,但其自身存在的局限性可能影响疗效和应用范围。因此急需开发新型药物或革新现有药物以提高IPC的疗效。近年来,纳米药物在腹腔注射中的试验研究为其提升化疗药物的疗效和降低不良反应带来新的临床应用前景[12],IPC技术与纳米药物的结合旨在将纳米医学的研究成果成功地应用于IPC的临床实践。
2 IPC的进展和应用
2.1 IPC的发展历程
IPC技术已从传统化疗药物转向新开发的药物,这些新型药物能够更有效地地穿透肿瘤细胞,提高局部药物浓度,同时减少全身毒性。目前,研究者们正在探索药物组合、优化给药方案和IPC技术,以提升腹膜转移癌的治疗效果。尽管IPC在一定程度上提高了疗效,但仍存在一些局限性,如药物可能无法达到杀灭所有肿瘤细胞的足够浓度、渗透能力有限、适用性问题及长期疗效有待进一步验证等,导致疗效不佳。
IPC的发展历程主要包括前期构建、早期探索、技术改进及临床应用等阶段(图1)。1744年,腹腔灌洗的想法首次被提出;接着,从20世纪50年代开始,人们尝试通过IPC来治疗腹腔内的恶性肿瘤[13];随后,腹腔导管技术的提出及不断改进提高了IPC的效率和安全性;最后, 1988年Fujimoto等[14]首次运用腹腔热灌注化疗(hyperthermic intraperitoneal chemotherapy, HIPEC)技术治疗胃肠恶性肿瘤后,IPC技术被广泛应用和推广,2000年Tempfer等[15]提出“化疗性气腹”的创新理念,2011年德国率先采用腹腔加压气溶胶(pressurized intraperitoneal aerosol chemotherapy,PIPAC)技术[16]。这些技术革新使IPC成为某些腹腔内恶性肿瘤的标准治疗手段之一[17-18]。
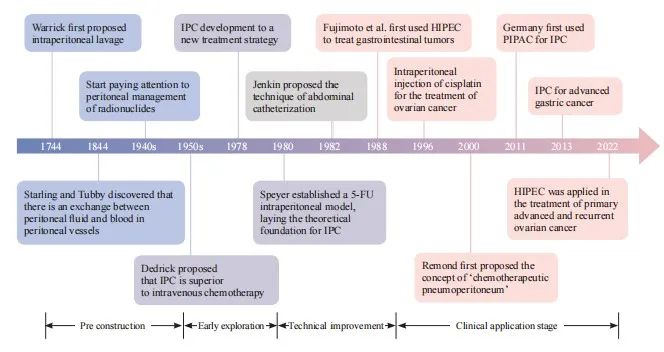
图1 IPC的临床治疗发展历程
Fig. 1 Clinical therapeutic developments of IPC
2.2 IPC技术的研究进展
IPC技术包括HIPEC、PIPAC等[19],可用于治疗PMP[20-22]和各种腹膜受累的晚期癌症(如肝细胞癌[23-24]、胆管癌[25]、胰腺癌[26]、胃癌[27]、妇科肿瘤[27]及其他腹部罕见癌症[28- 29])。
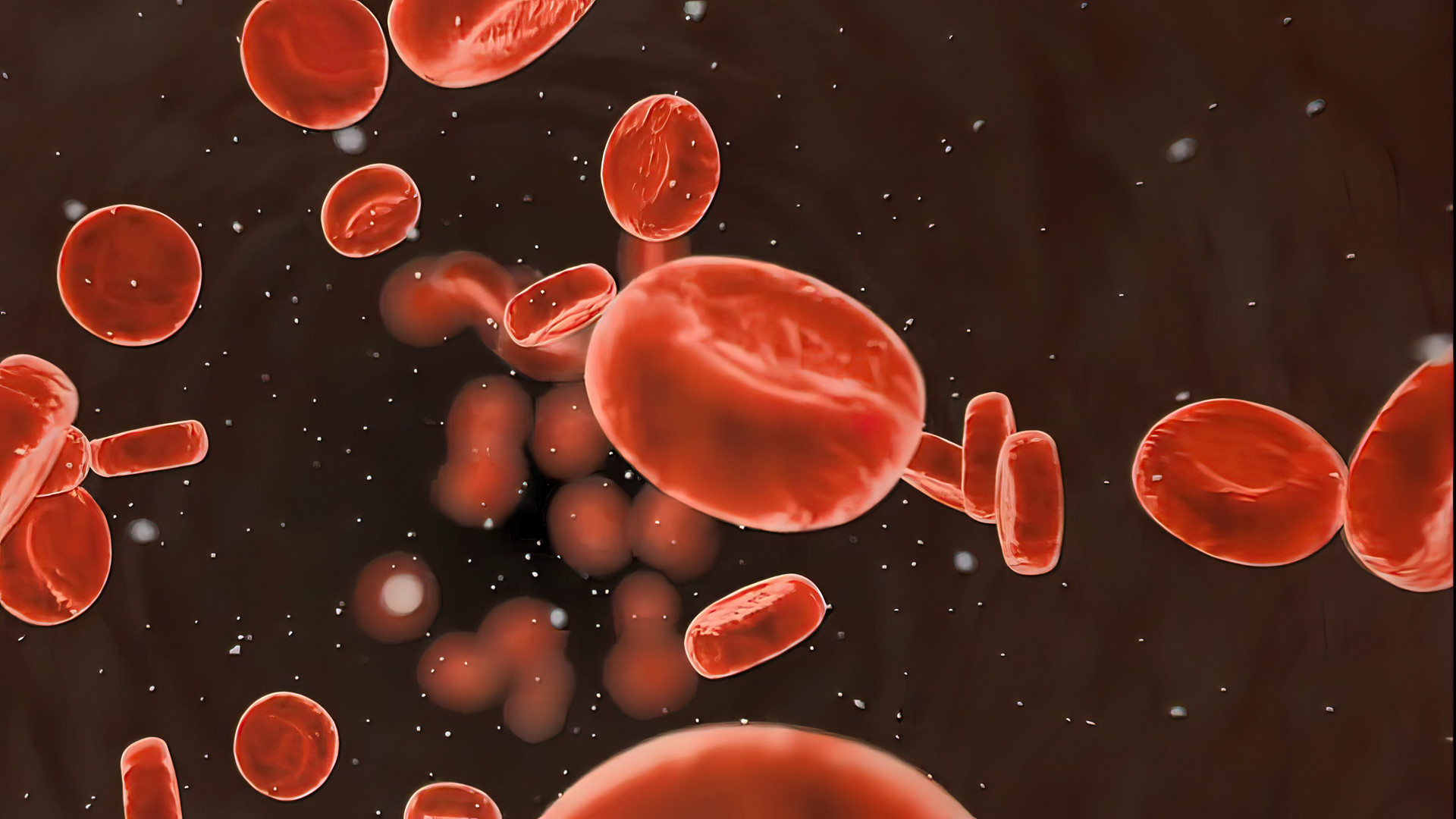
HIPEC和PIPAC等技术的引入显著提高了IPC的疗效。HIPEC将含化疗药物的灌注液加热至治疗温度(43 ℃),然后以恒定温度和循环方式注入患者的腹腔内,并维持一定的时间(60~120 min)[30]。通过化疗药物与热疗的协同增敏作用以及灌注液的循环冲刷作用,能够有效地杀灭和清除残留癌细胞及微小病灶,从而实现对肿瘤的局部控制并减缓疾病恶化[8,31](图2)。PIPAC作为一种新型局部给药技术,不与细胞减灭术(cytoreductive surgery,CRS)联合应用,PIPAC是在腹腔镜系统产生的高压下,通过雾化装置将化疗药物以加压气溶胶形式递送至腹腔内[32]。PIPAC的优势在于微创通路,较高局部浓度的化疗药物在腹膜内均匀分布、更深入地渗透到肿瘤组织中,而且极少会发生不良反应。PIPAC已在全球多个国家开展了大量相关的前瞻性研究和临床试验[32-33],结果均显示,PIPAC在各种腹膜转移癌患者中展现出良好的安全性和耐受性。
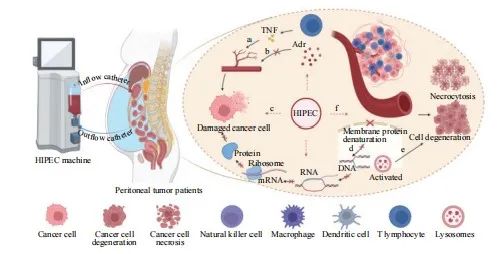
图2 HIPEC的温热效应
Fig. 2 The warm effect of HIPEC
a: TNF selectively disrupts blood vessels within tumor tissue, leading to thrombosis and ischemic necrosis. b: Tumor tissue, when exposed to heat stimuli, cannot regulate vasodilation via Adr, resulting in increased blood flow that fails to achieve thermoregulation. c: Cancer cells in the S/M phase are sensitive to hyperthermia, which induces cell death. d: Hyperthermia causes denaturation of membrane proteins, disrupting the synthesis of DNA, RNA and proteins. e: Heat stress activates lysosomes, causing cytoplasmic and nuclear damage, ultimately leading to cell apoptosis. f: Hyperthermia can trigger the immune system by activating heat shock proteins, stimulating various immune cells, including natural killer cells, macrophages, dendritic cells and T lymphocytes. This process inhibits angiogenesis, causing hypoxia, acidosis or nutrient deprivation, leading to cellular degeneration and necrosis. TNF: Tumor necrosis factor; Adr: Adrenaline. Created with BioRender.com.
2.3 IPC的临床应用
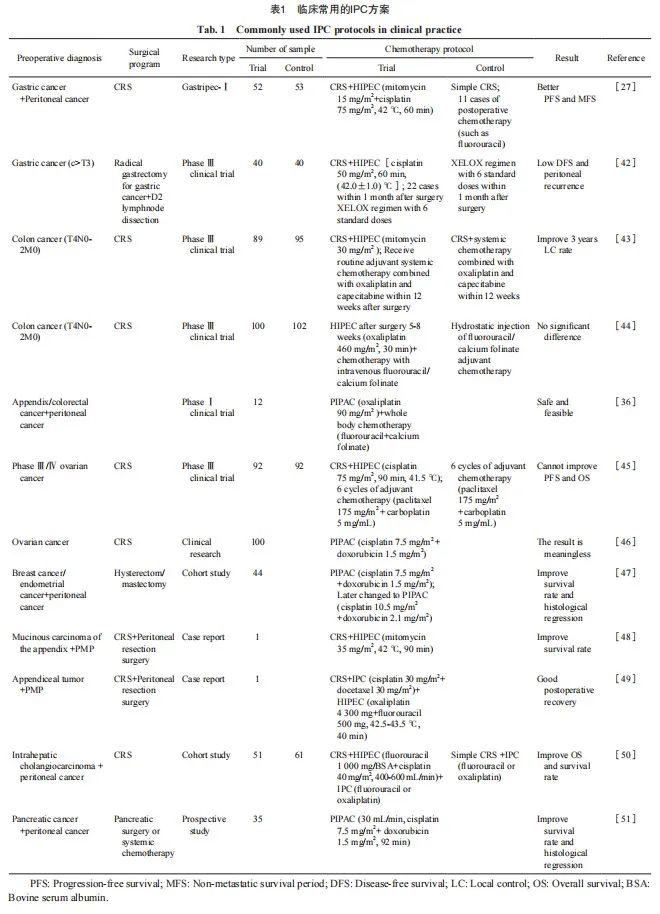
IPC可以提高药物的靶向性,减少药物在非靶部位的分布并降低药物引起的全身不良反应,因此常被用于将化疗药物递送至腹膜转移癌患者体内[34]。目前临床用于IPC的药物包括铂类药物[35-36]、紫杉醇[37]、5-氟尿嘧啶[38]、吉西他滨[39]、多柔比星[40]及丝裂霉素[41]等单一或联合用药,临床常用的IPC方案见表1。
2.3.1 IPC与胃癌
晚期胃癌患者极易发生腹膜转移,晚期胃癌的腹膜转移是导致患者死亡的重要因素[52]。一项回顾性多中心研究[53]结果表明,对于局限性和可切除性的腹膜转移癌患者,CRS联合HIPEC的治疗策略有利于提高患者的生存率;对于不可切除的腹膜转移癌患者,姑息性IPC的疗效更好[54]。然而,与单纯CRS相比,尽管CRS联合基于顺铂和丝裂霉素-C的HIPEC可显著改善无进展生存期(progression-free survival,PFS),但未改善总生存期(overall survival,OS)[27]。因此,HIPEC在胃癌腹膜转移患者治疗中的确切作用仍需进一步研究。
2.3.2 IPC与结直肠癌
相比于CRS术后单独全身化疗,联合全身化疗和基于丝裂霉素-C的HIPEC可以显著延长患者的局部控制时间(97.6个月 vs 87.6个月,P=0.03)[43]。然而,接受CRS后行IPC的患者与仅接受全身化疗患者的5年OS率无显著差异(69.6% vs 70.9%,P=0.692)[44]。鉴于上述研究结果的不一致性及PRODIGE 7研究[55]结果, HIPEC在结直肠癌腹膜转移癌中的作用还存在争议。对于PIPAC,也已有Ⅰ期临床试验[36]证实了奥沙利铂用于结直肠癌和阑尾癌腹膜转移的安全性和可行性。
2.3.3 IPC与妇科肿瘤
妇科肿瘤具有腹膜播散倾向,治疗常采用CRS联合化疗。然而,根治性手术与规范化疗后多数患者仍可能复发,并常因恶性肠梗阻而死亡。根据现有的美国国立综合癌症网络(National Comprehensive Cancer Network, NCCN)临床指南[56],对于接受CRS的Ⅲ期卵巢癌患者,推荐使用顺铂进行HIPEC。Van Driel等[57]通过对245例Ⅲ期卵巢癌患者进行间歇性CRS联合HIPEC,证实了HIPEC在卵巢癌治疗中的有效性。经过10年随访,生存分析结果与之前基本保持一致,证实HIPEC能够显著改善卵巢癌初治患者的预后[58],然而,随后的研究[45]却未能重现这一结果。已有研究[46-47]结果显示, PIPAC在不同妇科肿瘤中的作用并不一致。
2.3.4 IPC与PMP
CRS联合HIPEC已被确立为PMP的标准治疗方案[59]。Chua等[60]进行的一项回顾性研究,纳入2 298例源自阑尾的PMP患者,结果显示,在接受CRS联合HIPEC后,63%的患者生存时间超过10年,然而以往PMP的10年生存率仅为32%。进一步研究[48-49]显示,临床上采用CRS联合HIPEC治疗阑尾源性PMP有显著的积极作用。
2.3.5 IPC与胆管癌及胰腺癌
有研究[50]显示,采用CRS+基于5-氟尿嘧啶和顺铂的HIPEC+术后以5-氟尿嘧啶或奥沙利铂为主的全身化疗的51例肝内胆管癌腹膜转移患者的中位OS为25.53个月,但是采用单纯CRS+术后全身化疗的61例肝内胆管癌腹膜转移患者的中位OS仅为11.17个月,证明HIPEC对此类患者有效。有研究[51]纳入35例胰腺癌腹膜转移患者,采用雾化状态的顺铂和多柔比星进行治疗,使肿瘤组织消退并可改善患者的生活质量。
2.4 IPC技术的局限性
尽管HIPEC和PIPAC等IPC技术均已纳入腹膜转移癌治疗的临床实践中,但研究结果呈现出不一致性。这种差异可能源自研究设计中的若干限制,包括样本量小、未根据疾病分期或初次/间歇性CRS等进行严格分层、化疗药物剂量不足以及治疗持续时间不足等。尽管存在这些局限性,所有相关研究仍为IPC的临床应用提供了初步实践结果。未来的研究应在已有成果的基础上,结合当前的临床指南和推荐治疗策略,对药物的使用方案和治疗持续时间等进行优化调整,以期进一步提升IPC的临床疗效。
此外,IPC技术本身也存在一定局限性,例如:① 单次腹腔给药后,肿瘤结节表面浸润的深度有限,降低了靶向递送效率和特异性[61];② IPC要求药物在腹膜腔内长时间保持活性,然而当前药物的药代动力学不佳;③ 尽管IPC一定程度上提高了局部药物浓度,但由于受到药物分布不均、腹腔粘连、肿瘤较大或位置较深、药物被快速吸收或代谢、药物剂量不足或给药方式不当、患者个体差异及肿瘤耐药等多种因素影响,药物往往难以达到足够的浓度来杀灭所有肿瘤细胞[62]。因此,需要开发新型药物或对现有药物进行革新,以提高IPC的治疗效果。
3 纳米药物在IPC中的创新应用
纳米药物在IPC中的应用已取得显著进展,通过提高药物在腹腔内的靶向性、延长药物滞留时间及控制药物释放等,这些纳米药物可以有效地增强IPC的效果[63]。
3.1 纳米药物的基本原理及优势
首先,纳米药物的尺寸通常在1~100 nm之间,这种微小尺寸使它们能够更容易地穿透肿瘤组织,并利用肿瘤血管的通透性增强和滞留效应更有效地积聚在肿瘤部位[64-65]。其次,纳米药物可以通过物理包封和化学结合载药,药物在腹腔内有更好的稳定性和持续释放特性,以确保药物在病灶内长时间起效,减少在正常组织中的药物浓度进而减少不良反应。此外,纳米药物可以通过表面修饰特异性配体或抗体,来靶向肿瘤细胞或特定的肿瘤微环境,从而提高治疗的靶向性,减少对健康组织的损害。在IPC中,纳米药物通过其独特的物理和化学特性,提供了一种增强化疗效果、降低全身毒性的创新方式[66]。
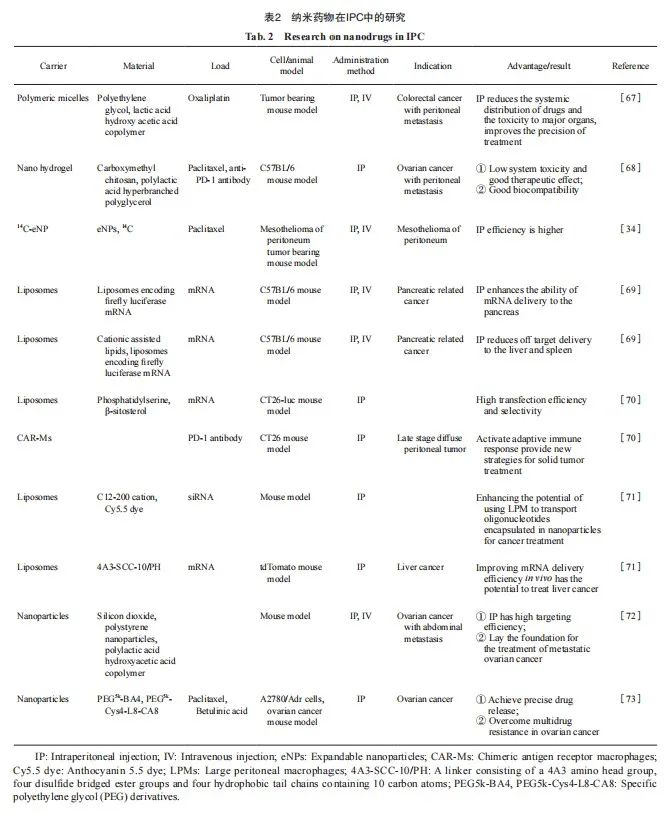
3.2 纳米药物的创新开发及应用
多种纳米药物载体系统在IPC研究中应用于多种腹膜转移癌模型中,主要包括聚合物胶束[67]、纳米水凝胶[68]、脂质体[69-71]和纳米粒子[72-73]等(表2)。这些纳米载体主要通过腹腔注射方式递送化疗药物、mRNA或抗体,用于治疗结直肠癌、卵巢癌、胰腺癌、肝癌及腹膜间皮瘤等。纳米载体的应用具有显著优势,包括降低系统毒性、提高药物靶向性、增强递送效率、延长药物滞留时间及克服肿瘤耐药性等。这些研究为进一步开发纳米药物用于IPC提供了重要的实验依据。此外,这些创新的纳米载药技术可以显著提高药物在体内的稳定性,降低药物的全身毒性,为腹膜转移癌的治疗提供更安全有效的选择[74]。
纳米载体凭借其独特尺寸和性能,能够有效地增强药物的靶点递送效率,并最大限度地减少脱靶风险[75]。在癌症治疗中,纳米材料通过功能化能够实现药物的靶向运输和联合治疗并显著提高疗效[76]。尽管纳米药物尚未广泛应用于临床,但这些研究为腹腔内肿瘤的靶向治疗奠定了基础,推动了纳米疗法向临床应用的转化。
4 挑战与展望
目前,IPC已被广泛用于治疗腹膜转移癌, HIPEC和PIPAC等技术也可显著改善腹膜转移癌患者的预后,延长生存期。然而,在临床中对于腹膜转移癌的治疗仍没有形成一套完整、规范的体系,在给药方式、药物类型和剂量、最终疗效等方面存在差异。尽管已经制定了基于循证医学证据的指南和推荐治疗策略,然而部分指南作为国外的证据评价体系,因种族差异并不适合直接应用于国内,迫切需要更多的临床试验和更高级别的循证医学证据,以更好地指导中国临床实践。
纳米颗粒凭借其亚微米尺寸、多功能特性和可调表面,可以穿透屏障将药物精准递送至癌细胞,从而显著增强化疗效果。尽管纳米药物在腹膜转移癌的治疗中显示出巨大潜力,但其开发和应用仍面临诸多挑战。未来的研究应优化纳米药物的设计和制备,明确其在体内的药代动力学和药效学特性,并评估其在临床应用中的安全性和有效性。此外,还需探索IPC与纳米药物的联合应用,并结合手术、放疗等其他治疗手段,以确立更全面、更个性化的腹膜转移癌治疗策略。
利益冲突声明:所有作者均声明不存在利益冲突。
作者贡献声明:
冯欣滢:参与文献调研,文章撰写及修改;王冰:参与讨论及文章修改;
刘培峰:指导文章选题,审阅文章知识性内容。
[参考文献]
[1] 中国抗癌协会腹膜肿瘤专业委员会. 中国肿瘤整合诊治指南:腹膜肿瘤(胃肠肿瘤部分)[J]. 消化肿瘤杂志(电子版), 2023, 15(2): 100-108.
Chinese Society of Peritoneal Oncology, China Anti-Cancer Association. China Anti-Cancer Association guidelines for holistic integrative management of cancer-peritoneal tumours from gastrointestinal tract[J]. J Digest Oncol (Elect Ver), 2023, 15(2): 100-108.
[2] 唐鸿生, 阮 强, 崔书中. 《中国肿瘤整合诊治指南: 腹膜肿瘤》解读[J]. 消化肿瘤杂志(电子版), 2023, 15(2): 109-113.
TANG H S, RUAN Q, CUI S Z. Interpretation of China Anti- Cancer Association (CACA) guidelines for holistic integrative management of cancer-peritoneal tumours[J]. J Digest Oncol (Elect Ver), 2023, 15(2): 109-113.
[3] LEI Z Y, WANG J H, LI Z, et al. Hyperthermic intraperitoneal chemotherapy for gastric cancer with peritoneal metastasis: a multicenter propensity score-matched cohort study[J]. Chin J Cancer Res, 2020, 32(6): 794-803.
[4] 关天培, 雷子颖, 崔书中. 结肠直肠癌腹膜转移防治临床研究[J]. 外科理论与实践, 2021, 26(1): 7-10.
GUAN T P, LEI Z Y, CUI S Z. Clinical study on prevention and treatment of peritoneal metastasis of colorectal cancer[J]. J Surg Concepts Pract, 2021, 26(1): 7-10.
[5] 樊代明, 崔书中. 中国肿瘤整合诊治指南:腹膜肿瘤(2022)[M]. 天津科学技术出版社, 2022.
FAN D M, CUI S Z. Guidelines for integrated diagnosis and treatment of tumors in china: peritoneal tumors (2022)[M]. Tianjin Sci Technol Press, 2022.
[6] HOSSAIN M B, HALDAR NEER A H. Chemotherapy[M]//QAZI A S, TARIQ K. Therapeutic approaches in cancer treatment: vol. 185. Berlin: Springer, 2023: 49-58.
[7] JACQUET P, SUGARBAKER P H. Peritoneal-plasma barrier[M]//SUGARBAKER P H. Peritoneal carcinomatosis: principles of management. Berlin: Springer, 1996: 53-63.
[8] SADEGHI B, ARVIEUX C, GLEHEN O, et al. Peritoneal carcinomatosis from non-gynecologic malignancies: results of the EVOCAPE 1 multicentric prospective study[J]. Cancer, 2000, 88(2): 358-363.
[9] JAABACK K, JOHNSON N, LAWRIE T A. Intraperitoneal chemotherapy for the initial management of primary epithelial ovarian cancer[J]. Cochrane Database Syst Rev, 2016, 2016(1): CD005340.
[10] CARLIER C, MATHYS A, JAEGHERE E D, et al. Tumour tissue transport after intraperitoneal anticancer drug delivery[J]. Int J Hyperthermia, 2017, 33(5): 534-542.
[11] GUCHELAAR N A D, NASSERINEJAD K, MOSTERT B, et al. Intraperitoneal chemotherapy for peritoneal metastases of gastric origin: a systematic review and meta-analysis[J]. Br J Surg, 2024, 111(5): znae116.
[12] SHI J J, KANTOFF P W, WOOSTER R, et al. Cancer nanomedicine: progress, challenges and opportunities[J]. Nat Rev Cancer, 2017, 17(1): 20-37.
[13] AL-QUTEIMAT O M, AL-BADAINEH M A. Intraperitoneal chemotherapy: rationale, applications, and limitations[J]. J Oncol Pharm Pract, 2014, 20(5): 369-380.
[14] FUJIMOTO S, SHRESTHA R D, KOKUBUN M, et al. Intraperitoneal hyperthermic perfusion combined with surgery effective for gastric cancer patients with peritoneal seeding[J]. Ann Surg, 1988, 208(1):36-41.
[15] TEMPFER C B, SOLASS W, REYMOND M A. Pressurized intraperitoneal chemotherapy (PIPAC) in women with gynecologic malignancies: a review[J]. Wien Med Wochenschr, 2014, 164(23/24): 519-528.
[16] SOLASS W, KERB R, MÜRDTER T, et al. Intraperitoneal chemotherapy of peritoneal carcinomatosis using pressurized aerosol as an alternative to liquid solution: first evidence for efficacy[J]. Ann Surg Oncol, 2014, 21(2): 553-559.
[17] COCCOLINI F, COTTE E, GLEHEN O, et al. Intraperitoneal chemotherapy in advanced gastric cancer. Meta-analysis of randomized trials[J]. Eur J Surg Oncol, 2014, 40(1): 12-26.
[18] FILIS P, MAURI D, MARKOZANNES G, et al. Hyperthermic intraperitoneal chemotherapy (HIPEC) for the management of primary advanced and recurrent ovarian cancer: a systematic review and meta-analysis of randomized trials[J]. ESMO Open, 2022, 7(5): 100586.
[19] CORTÉS-GUIRAL D, HÜBNER M, ALYAMI M, et al. Primary and metastatic peritoneal surface malignancies[J]. Nat Rev Dis Primers, 2021, 7(1): 91.
[20] SANTULLO F, PACELLI F, ABATINI C, et al. Cytoreduction and hyperthermic intraperitoneal chemotherapy for pseudomyxoma peritonei of appendiceal origin: a single center experience[J]. Front Surg, 2021, 8: 715119.
[21] KUSAMURA S, BARRETTA F, YONEMURA Y, et al. The role of hyperthermic intraperitoneal chemotherapy in pseudomyxoma peritonei after cytoreductive surgery[J]. JAMA Surg, 2021, 156(3): e206363.
[22] PAPANTONI E, NTATSIS K, KYZIRIDIS D, et al. Twentyyears’ experience with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) for pseudomyxoma peritonei (PMP)[J]. J BUON, 2021, 26(4): 1647-1652.
[23] MAJEED A, ALAPARTHI S, HALEGOUA-DEMARZIO D, et al. Complete pathologic response to gemcitabine and oxaliplatin chemotherapy after prior therapies in a patient with hepatocellular carcinoma and peritoneal metastases undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy[J]. World J Oncol, 2024, 15(3): 511-520.
[24] HUNG K C, YANG K L, HUANG G C, et al. Cytoreduction surgery and hyperthermic intraperitoneal chemotherapy for treating advanced peritoneal metastases of hepatocellular carcinoma[J]. Pleura Peritoneum, 2020, 5(2): 20190030.
[25] HERNANDEZ D L, RESTREPO J, GARCIA MORA M. Peritoneal metastasis of cholangiocarcinoma treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy at the instituto nacional de cancerología, Colombia[J]. Cureus, 2020, 12(1): e6697.
[26] FRASSINI S, CALABRETTO F, GRANIERI S, et al. Intraperitoneal chemotherapy in the management of pancreatic adenocarcinoma: a systematic review and meta-analysis[J]. Eur J Surg Oncol, 2022, 48(9): 1911-1921.
[27] RAU B, LANG H, KOENIGSRAINER A, et al. Effect of hyperthermic intraperitoneal chemotherapy on cytoreductive surgery in gastric cancer with synchronous peritoneal metastases: the phase Ⅲ GASTRIPEC-I trial[J]. J Clin Oncol, 2024, 42(2): 146-156.
[28] LIU G, JI Z H, YU Y, et al. Treatment of hypermyoglobinemia after CRS+HIPEC for patients with peritoneal carcinomatosis: a retrospective comparative study[J]. Medicine, 2017, 96(45): e8573.
[29] BRANDL A, ZIELINSKI C B, RAUE W, et al. Peritoneal metastases of rare carcinomas treated with cytoreductive surgery and HIPEC-a single center case series[J]. Ann Med Surg, 2017, 22: 7-11.
[30] GLEHEN O, MOHAMED F, GILLY F N. Peritoneal carcinomatosis from digestive tract cancer: new management by cytoreductive surgery and intraperitoneal chemohyperthermia[J]. Lancet Oncol, 2004, 5(4): 219-228.
[31] FRIEDRICH M, ZINN W, KOLNSBERG L, et al. Hyperthermic intraperitoneal chemotherapy (HIPEC) for ovarian cancer: evaluation of side effects in a single institution cohort[J]. Anticancer Res, 2020, 40(3): 1481-1486.
[32] ALYAMI M, HÜBNER M, GRASS F, et al. Pressurised intraperitoneal aerosol chemotherapy: rationale, evidence, and potential indications[J]. Lancet Oncol, 2019, 20(7): e368-e377.
[33] GUEL-KLEIN S, ALBERTO VILCHEZ M E, CEELEN W, et al. Is PIPAC a treatment option in upper and lower gastrointestinal cancer with peritoneal metastasis?[J]. Visc Med, 2022, 38(2): 90-98.
[34] COLBY A H, KIRSCH J, PATWA A N, et al. Radiolabeled biodistribution of expansile nanoparticles: intraperitoneal administration results in tumor specific accumulation[J]. ACS Nano, 2023, 17(3): 2212-2221.
[35] MOUKARZEL L A, FERRANDO L, DOPESO H, et al. Hyperthermic intraperitoneal chemotherapy (HIPEC) with carboplatin induces distinct transcriptomic changes in ovarian tumor and normal tissues[J]. Gynecol Oncol, 2022, 165(2): 239-247.
[36] RAOOF M, WHELAN R L, SULLIVAN K M, et al. Safety and efficacy of oxaliplatin pressurized intraperitoneal aerosolized chemotherapy (PIPAC) in colorectal and appendiceal cancer with peritoneal metastases: results of a multicenter phase Ⅰ trial in the USA[J]. Ann Surg Oncol, 2023, 30(12): 7814-7824.
[37] ZHANG Y M, WANG S L, DUAN X F, et al. mPEG-PDLLA micelles potentiate docetaxel for intraperitoneal chemotherapy in ovarian cancer peritoneal metastasis[J]. Front Pharmacol, 2022, 13: 861938.
[38] SHIMIZU T, SONODA H, MURATA S, et al. Hyperthermic intraperitoneal chemotherapy using a combination of mitomycin C, 5-fluorouracil, and oxaliplatin in patients at high risk of colorectal peritoneal metastasis: a phase Ⅰ clinical study[J]. Eur J Surg Oncol, 2014, 40(5): 521-528.
[39] SUGARBAKER P H. Optimizing regional chemotherapy for epithelial ovarian cancer[J]. J Obstet Gynaecol Res, 2022, 48(6): 1306-1317.
[40] NADIRADZE G, GIGER-PABST U, ZIEREN J, et al. Pressurized intraperitoneal aerosol chemotherapy (PIPAC) with low-dose cisplatin and doxorubicin in gastric peritoneal metastasis[J]. J Gastrointest Surg, 2016, 20(2): 367-373.
[41] HELDERMAN R F C P A, LÖKE D R, VERHOEFF J, et al. The temperature-dependent effectiveness of platinumbased drugs mitomycin-C and 5-FU during hyperthermic intraperitoneal chemotherapy (HIPEC) in colorectal cancer cell lines[J]. Cells, 2020, 9(8): 1775.
[42] BEEHARRY M K, ZHU Z L, LIU W T, et al. Prophylactic HIPEC with radical D2 gastrectomy improves survival and peritoneal recurrence rates for locally advanced gastric cancer: Personal experience from a randomized case control study[J]. BMC Cancer, 2019, 19(1): 932.
[43] ARJONA-SÁNCHEZ A, ESPINOSA-REDONDO E, GUTIÉRREZ-CALVO A, et al. Efficacy and safety of intraoperative hyperthermic intraperitoneal chemotherapy for locally advanced colon cancer: a phase 3 randomized clinical trial[J]. JAMA Surg, 2023, 158(7): 683-691.
[44] ZWANENBURG E S, KLAVER C E, WISSELINK D D, et al. Adjuvant hyperthermic intraperitoneal chemotherapy in patients with locally advanced colon cancer (COLOPEC): 5-year results of a randomized multicenter trial[J]. J Clin Oncol, 2024, 42(2): 140-145.
[45] LIM M C, CHANG S J, PARK B, et al. Survival after hyperthermic intraperitoneal chemotherapy and primary or interval cytoreductive surgery in ovarian cancer: a randomized clinical trial[J]. JAMA Surg, 2022, 157(5): 374-383.
[46] TALIENTO C, RESTAINO S, SCUTIERO G, et al. Pressurized intraperitoneal aerosol chemotherapy (PIPAC) with cisplatin and doxorubicin in patients with ovarian cancer: a systematic review[J]. Eur J Surg Oncol, 2023, 49(12): 107250.
[47] REZNICZEK G A, GIGER-PABST U, THAHER O, et al. Pressurized intraperitoneal aerosol chemotherapy (PIPAC) for rare gynecologic indications: peritoneal metastases from breast and endometrial cancer[J]. BMC Cancer, 2020, 20(1): 1122.
[48] AWAD A, AWAD M, ALAMI M, et al. Successful treatment of pseudomyxoma peritonei (PMP) through cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (CRS-HIPEC): a case report and literature review[J]. Int J Surg Case Rep, 2024, 119: 109656.
[49] PADMANABHAN N, ISHIBASHI H, NISHIHARA K, et al. Complete pathological response of high grade appendicular neoplasm induced pseudomyxoma peritonei (PMP) after neoadjuvant intra-peritoneal chemotherapy: a case report[J]. Int J Surg Case Rep, 2020, 72: 117-121.
[50] FENG F L, GAO Q X, WU Y, et al. Cytoreductive surgery combined with hyperthermic intraperitoneal chemotherapy vs cytoreductive surgery alone for intrahepatic cholangiocarcinoma with peritoneal metastases: a retrospective cohort study[J]. Eur J Surg Oncol, 2021, 47(9): 2363-2368.
[51] KRYH-JENSEN C G, FRISTRUP C W, AINSWORTH A P, et al. What is long-term survival in patients with peritoneal metastasis from gastric, pancreatic, or colorectal cancer? A study of patients treated with systemic chemotherapy and pressurized intraperitoneal aerosol chemotherapy (PIPAC)[J]. Pleura Peritoneum, 2023, 8(4): 147-155.
[52] JI Z H, PENG K W, YU Y, et al. Current status and future prospects of clinical trials on CRS+HIPEC for gastric cancer peritoneal metastases[J]. Int J Hyperthermia, 2017, 33(5): 562-570.
[53] GLEHEN O, GILLY F N, ARVIEUX C, et al. Peritoneal carcinomatosis from gastric cancer: a multi-institutional study of 159 patients treated by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy[J]. Ann Surg Oncol, 2010, 17(9): 2370-2377.
[54] [54] LÓPEZ-BASAVE H N, QUIROZ-SANDOVAL O A, PADILLA-ROSCIANO A E, et al. Papel de la cirugía citorreductora y la quimioterapia intraperitoneal hipertérmica en el tratamiento del cáncer gástrico[J]. Cirugía Y Cirujanos, 2019, 86(3): 936.
[55] QUÉNET F, ELIAS D, ROCA L, et al. Cytoreductive surgery plus hyperthermic intraperitoneal chemotherapy versus cytoreductive surgery alone for colorectal peritoneal metastases (PRODIGE 7): a multicentre, randomised, open label, phase 3 trial[J]. Lancet Oncol, 2021, 22(2): 256-266.
[56] National Comprehensive Cancer Network. NCCN guideline in ovarian cancer/fallopian tube cancer/primary peritoneal cancer (version 1. 2022) [EB/OL]. (2022-03-02)[2024-07-31]. http://www,nccn,org/professionals/physician gls/pdf/ovarian.pdf.
[57] VAN DRIEL W J, KOOLE S N, SIKORSKA K, et al. Hyperthermic intraperitoneal chemotherapy in ovarian cancer[J]. N Engl J Med, 2018, 378(3): 230-240.
[58] ARONSON S L, LOPEZ-YURDA M, KOOLE S N, et al. Cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy in patients with advanced ovarian cancer (OVHIPEC-1): final survival analysis of a randomised, controlled, phase 3 trial[J]. Lancet Oncol, 2023, 24(10): 1109-1118.
[59] SUGARBAKER P H. New standard of care for appendiceal epithelial neoplasms and pseudomyxoma peritonei syndrome?[J]. Lancet Oncol, 2006, 7(1): 69-76.
[60] CHUA T C, MORAN B J, SUGARBAKER P H, et al. Earlyand long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy[J]. J Clin Oncol, 2012, 30(20): 2449-2456.
[61] SUGARBAKER P H, VAN DER SPEETEN K. Surgical technology and pharmacology of hyperthermic perioperative chemotherapy[J]. J Gastrointest Oncol, 2016, 7(1): 29-44.
[62] B R E U S A S , Z I L I O S , C A T A N I A G , e t a l . L o c a l i z e d chemotherapy approaches and advanced drug delivery strategies: a step forward in the treatment of peritoneal carcinomatosis from ovarian cancer[J]. Front Oncol, 2023, 13: 1125868.
[63] LAGAST N, CARLIER C, CEELEN W P. Pharmacokinetics and tissue transport of intraperitoneal chemotherapy[J]. Surg Oncol Clin N Am, 2018, 27(3): 477-494.
[64] MATSUMURA Y, MAEDA H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs[J]. Cancer Res, 1986, 46(12 Pt 1): 6387-6392.
[65] SMET L D, CEELEN W, REMON J P, et al. Optimization of drug delivery systems for intraperitoneal therapy to extend the residence time of the chemotherapeutic agent[J]. Sci World J, 2013, 2013: 720858.
[66] WANG X H, ZHANG H, CHEN X H, et al. Overcoming tumor microenvironment obstacles: current approaches for boosting nanodrug delivery[J]. Acta Biomater, 2023, 166: 42-68.
[67] SUN T, ZHANG G P, NING T T, et al. A versatile theranostic platform for colorectal cancer peritoneal metastases: real-time tumor-tracking and photothermal-enhanced chemotherapy[J]. Adv Sci, 2021, 8(20): e2102256.
[68] LIANG S, XIAO L Y, CHEN T, et al. Injectable nanocomposite hydrogels improve intraperitoneal co-delivery of chemotherapeutics and immune checkpoint inhibitors for enhanced peritoneal metastasis therapy[J]. ACS Nano, 2024, 18(29): 18963-18979.
[69] MELAMED J R, YERNENI S S, ARRAL M L, et al. Ionizable lipid nanoparticles deliver mRNA to pancreatic β cells via macrophage-mediated gene transfer[J]. Sci Adv, 2023, 9(4): eade1444.
[70] GU K, LIANG T, HU L, et al. Intraperitoneal programming of tailored CAR macrophages via mRNA-LNP to boost cancer immunotherapy[M/OL]. (2024-07-30)[2024-08-26]. http://biorxiv.org/lookup/doi/10.1101/2024.07.30.605730.
[71] CHEN Z M, TIAN Y, YANG J Y, et al. Modular design of biodegradable ionizable lipids for improved mRNA delivery and precise cancer metastasis delineation in vivo[J]. J Am Chem Soc, 2023, 145(44): 24302-24314.
[72] HABER T, CORNEJO Y R, ARAMBURO S, et al. Specific targeting of ovarian tumor-associated macrophages by large, anionic nanoparticles[J]. Proc Natl Acad Sci U S A, 2020, 117(33): 19737-19745.
[73] QU H J, YANG J F, LI S J, et al. Programmed-response crosslinked nanocarrier for multidrug-resistant ovarian cancer treatment[J]. J Control Release, 2023, 357: 274-286.
[74] WANG K, SHEN R Y, MENG T T, et al. Nano-drug delivery systems based on different targeting mechanisms in the targeted therapy of colorectal cancer[J]. Molecules, 2022, 27(9): 2981.
[75] HAN X J, GONG C N, YANG Q R, et al. Biomimetic nanodrug delivery system: an emerging platform for promoting tumor treatment[J]. Int J Nanomedicine, 2024, 19: 571-608.
[76] ZAIKI Y, ISKANDAR A, WONG T W. Functionalized chitosan for cancer nano drug delivery[J]. Biotechnol Adv, 2023, 67: 108200.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#靶向治疗# #纳米药物# #腹膜转移癌# #腹腔热灌注化疗# #腹腔化疗# #腹腔加压气溶胶#
15