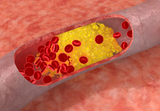
J Neuroophthalmol:血管钙化导致前叶缺血性视神经病变!
2017-10-19 cuiguizhong MedSci原创
挪威奥斯陆大学医院眼科的Sivertsen MS 近日在J Neuroophthalmol杂志上发表了他们近期的一项工作,题目为"Anterior Ischemic Optic Neuropathy Due to Calciphylaxis",报道了一名72岁的女性患者,她的左眼患有前叶缺血性视神经病变。
挪威奥斯陆大学医院眼科的Sivertsen MS 近日在J Neuroophthalmol杂志上发表了他们近期的一项工作,题目为"Anterior Ischemic Optic Neuropathy Due to Calciphylaxis",报道了一名72岁的女性患者,她的左眼患有前叶缺血性视神经病变。他们通过眼底荧光素血管造影的方法,发现明显的巨细胞性动脉炎症状。与血管钙化相似,颞动脉活检显示血管壁广泛钙化。因此,他们建议,在前叶局部缺血性视神经病变的鉴别诊断中,考虑到这种疾病的不寻常,应特别考虑动脉形态。这项工作为眼科临床医生完善前叶缺血性视神经病变的诊断提供了思路。原文出处:Sivertsen, M.S., E.H. Strom, and K.M.A. Endre, Anterior Ischemic Optic Neuropathy Due to Calciphylaxis. J Neuroophthalmol, 2017本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#视神经#
0
#缺血性#
29
#视神经病变#
24
#神经病#
20
#神经病变#
30
#THA#
32
好好文章学习了
56
学习了谢谢分享
49