Eur Urol:前列腺特异性膜抗原正电子发射断层扫描/计算机断层扫描成像对前列腺癌是否划算?
2020-12-31 AlexYnag MedSci原创
在将前列腺特异性膜抗原(PSMA)正电子发射断层扫描/计算机断层扫描(PET/CT)纳入常规护理之前,评估其效益是重要的。最近,有研究人员确定了PSMA-PET/CT与常规成像相比的效益情况。
在将前列腺特异性膜抗原(PSMA)正电子发射断层扫描/计算机断层扫描(PET/CT)纳入常规护理之前,评估其效益是重要的。最近,有研究人员确定了PSMA-PET/CT与常规成像相比的效益情况。
研究人员的效益分析包括了proPSMA研究中的数据,其中包括高风险前列腺癌患者,并分配到常规成像或68Ga-PSMA-11 PET/CT,并收集了预先计划的卫生经济学数据。结果表明,PSMA PET/CT每次扫描的估计成本为1203澳元,低于传统成像成本1412澳元。因此,PSMA PET/CT占主导地位,且具有更高的准确性和更低的成本。因此,可节省额外的准确检测结节性疾病的费用959澳元,以及准确检测远处转移的费用1412澳元。这些结果对每次68Ga-PSMA-11运行扫描的男性数量变化最为敏感。需要后续的研究来评估PSMA PET/CT指导护理的长期成本和效益。
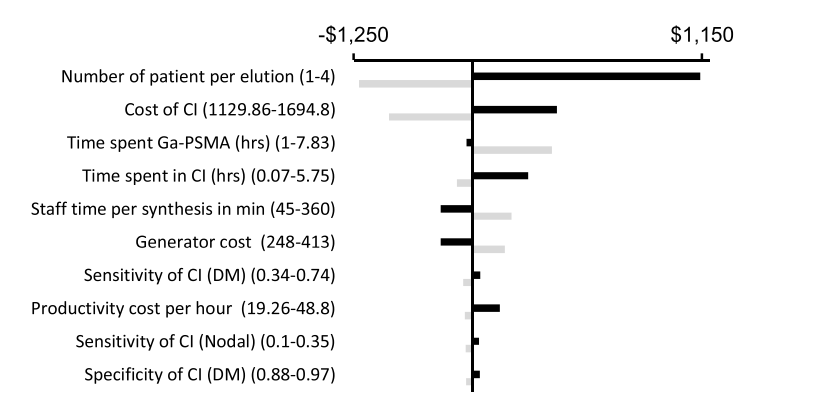
最后,研究人员指出,与传统成像相比,PSMA PET/CT对高风险前列腺癌男性的初始分期具有更低的直接比较成本和更高的准确性,为在临床实践中采用PSMA PET/CT提供了一个令人信服的理由。
原始出处:
Rafael E de Feria Cardet , Michael S Hofman , Tatiana Segard et al. Is Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography Imaging Cost-effective in Prostate Cancer: An Analysis Informed by the proPSMA Trial. Eur Urol. Dec 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#计算机#
51
#前列腺特异性膜抗原#
43
#特异性#
38
#抗原#
33
前列腺癌相关研究,学习了,谢谢梅斯
47