Diabetic Med:运动可保护新发1型糖尿病(EXTOD)患者的β-细胞功能?
2017-10-27 MedSci MedSci原创
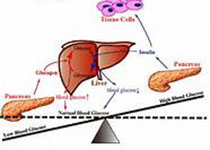
近日,国际杂志 《Diabetic Medicine》上在线发表一项关于运动可保护新发1型糖尿病(EXTOD)患者的β-细胞功能的随机对照试验性试验的研究。在诊断为1型糖尿病时残留的β细胞功能即会显现。保留这种β细胞功能可减少并发症。研究人员假设运动在1型糖尿病中可保护β细胞功能,并对此进行试点试验。
近日,国际杂志 《Diabetic
Medicine》上在线发表一项关于运动可保护新发1型糖尿病(EXTOD)患者的β-细胞功能的随机对照试验性试验的研究。在诊断为1型糖尿病时残留的β细胞功能即会显现。保留这种β细胞功能可减少并发症。研究人员假设运动在1型糖尿病中可保护β细胞功能,并对此进行试点试验。
研究人员开展了随机对照试验,研究纳入了在过去3个月内诊断为1型糖尿病的16-60岁成年人。参与者被分配到对照(常规护理)或干预(每月的锻炼咨询)组,以1:1的比例进行12个月的治疗。主要结果是招募率,中途退出,运动依从性(≥50分钟自我报告的中度至强烈体力活动(MVPA)],以及对照组的运动摄取。次要结局是6和12个月时胰岛素敏感性和干预、对照组之间β细胞功能丧失率的差异。
研究显示对最初的507人筛选后,58人(28人对照组,30人干预)进入研究,41人完成了本项研究。参与者主要是白色欧洲男性,BMI为24.8±3.8 kg / m 2,HbA 1c75±25 mmol / mol(9±2%)。干预组的平均MVPA水平升高(平均值243〜273 min /周),61%的干预参与者在本年度至少42周内达到自己报告的MVPA≥150 min /周的目标。对照组的体力活动水平略有下降(平均值为277〜235分钟,MVPA /周)。有探索证据表明干预组胰岛素敏感增加,需要较少的胰岛素。然而,各组之间β细胞功能的丧失率似乎相似,尽管胰岛素敏感性的变化可能影响了这一点。
研究表明,可以招募并随机分配新诊断的1型糖尿病患者进行锻炼干预试验,增加并维持其12个月运动水平。未来的试验需要采取更加能够坚持运动训练目标的措施,并包括使用更适当的β细胞功能的测量方法。
原始出处:
P. Narendran, N. Jackson, A. Daley,et al. You have free
access to this contentExercise to preserve β-cell function in recent-onset Type
1 diabetes mellitus (EXTOD) – a randomized controlled pilot trial
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#DIA#
17
不错
40
#BET#
26
#Diabetic#
26
#细胞功能#
31
#Med#
21
非常好的文章.谢谢
37