盘点:2月Cell杂志精选文章一览
2017-02-27 MedSci MedSci原创
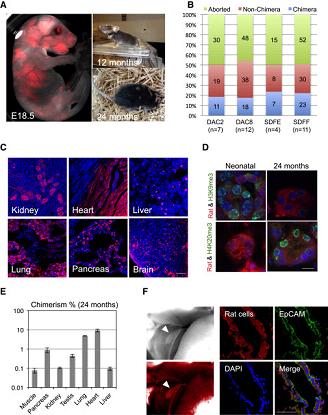
1月即将过去,Cell杂志就刊登了不少重量级研究,本文小编挑选了读者普遍关注的亮点研究,整理成文,分享给各位!【1】CELL:人类适应性免疫救援固有免疫的先天性错误 近期,一项发表在权威杂志CELL上的研究描述了八个与常染色体隐性TIRAP缺乏相关的个体。威胁生命的葡萄球菌疾病发生在儿童期,但不是在其他七个纯合子。在所有TIRAP缺陷个体的成纤维细胞和白细胞中,对所有Toll样受体1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
39
#Cell杂志#
44
#Cell#
36
感谢分享一下
71
感谢分享一下
57
这个还是非常有用的资料,每次都感觉很不错!
68
感谢分享一下
66
赞!
59
威胁生命的葡萄球菌疾病发生在儿童期。
33
获得性抗LTA Abs拯救了遗传性TIRAP缺乏的个体中TLR2依赖免疫的葡萄球菌LTA。
34