JAHA:血清生长分化因子15水平与缺血性卒中后抑郁相关
2022-01-03 MedSci原创 MedSci原创
缺血性卒中急性期血清GDF-15水平升高与PSD独立相关,表明GDF-15水平可能是PSD有价值的预后生物标志物。
卒中是导致死亡和长期残疾的主要原因,已成为全球重要的公共卫生问题。在卒中幸存者的所有并发症中,卒中后抑郁症(PSD)是最常见的精神问题。2005年,Hackett等人进行的一项系统评价估计了PSD的发生率高达33%(95%CI为29%-36%)。PSD引起的后果不仅限于心理健康;它还会对康复和生活质量产生不利影响,并增加患者卒中后死亡的风险。

但是血清生长分化因子15(GDF-15)对PSD的影响仍然未知。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究的目的是探讨缺血性卒中患者血清GDF-15水平与PSD之间的相关性。
该研究基于来自CATIS(中国急性缺血性卒中抗高血压试验)的随机样本,分析了来自7家参与医院的572名患者的GDF-15水平。研究结果是缺血性卒中后3个月出现的抑郁症状(汉密尔顿抑郁量表评分≥8)。
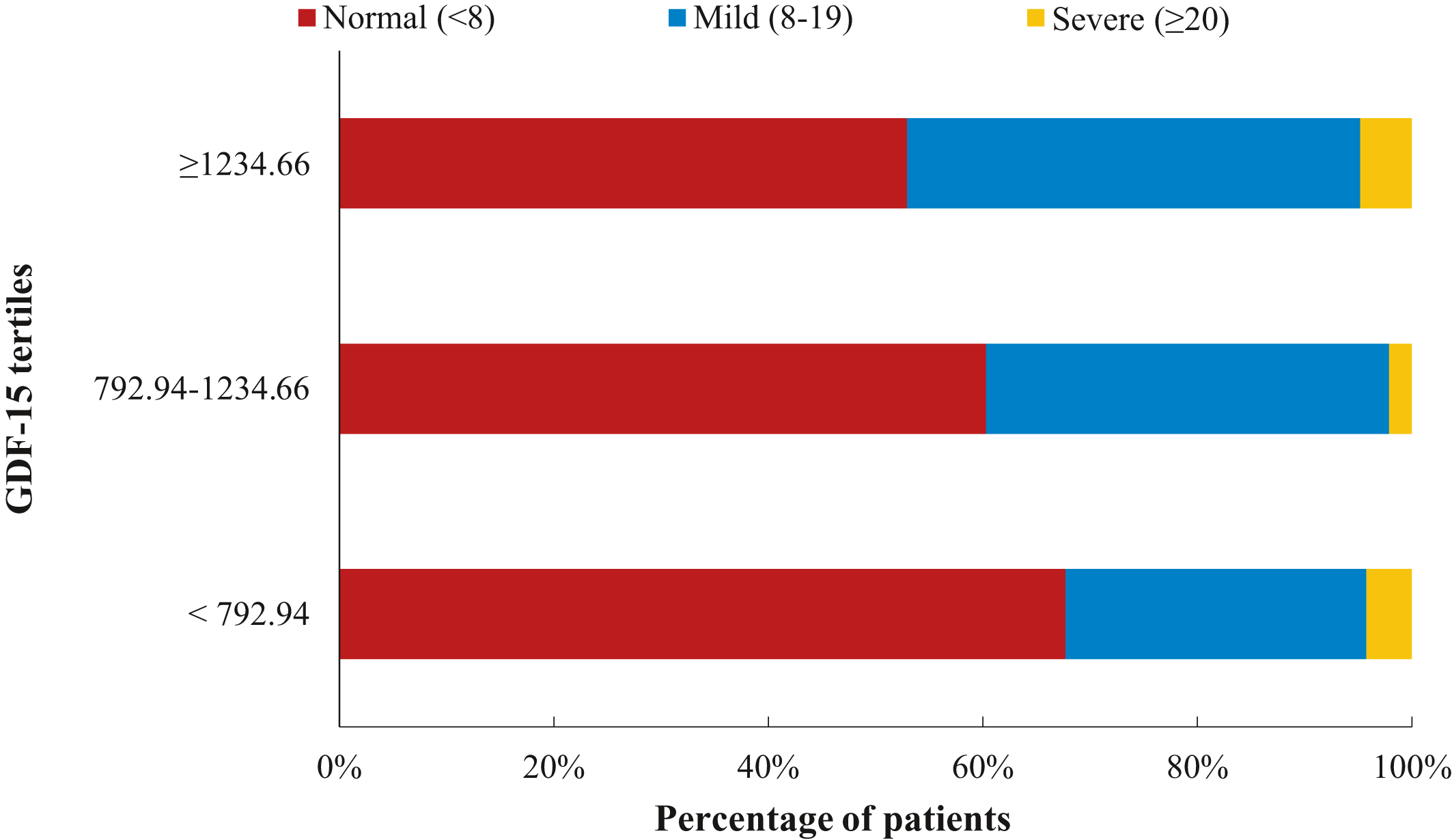
该研究共有231名(40.4%)卒中患者在3个月内经历了PSD。与最低三分位数相比,与血清GDF-15水平最高三分位数相关的PSD的多变量调整比值比为2.92(95%CI为1.36-6.27)。GDF-15水平对数转换后每增加1个SD与PSD风险增加42%(95%CI为2%-97%)相关,并且观察到血清GDF-15水平与PSD风险之间存在线性关联(线性P=0.006)。
由此可见,缺血性卒中急性期血清GDF-15水平升高与PSD独立相关,表明GDF-15水平可能是PSD有价值的预后生物标志物。
原始出处:
Yuhan Zang,et al.Serum Growth Differentiation Factor 15 Levels Are Associated With Depression After Ischemic Stroke.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.022607
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#生长分化因子15#
47
#卒中后#
29
#缺血性卒#
39
#缺血性#
33
#AHA#
33
感谢分享
46