NATURE:H +转运是线粒体ADP / ATP载体的整合功能
2019-07-27 海北 MedSci原创
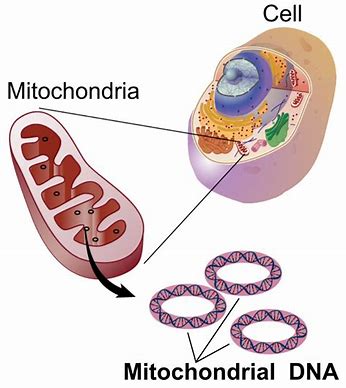
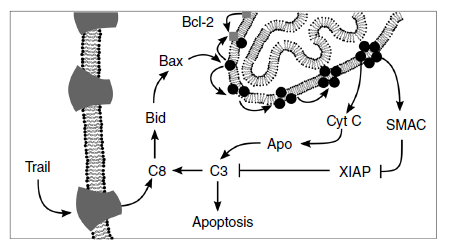
线粒体ADP / ATP载体(AAC)是线粒体内膜的主要转运蛋白。它交换线粒体ATP和细胞溶质ADP,并控制ATP的细胞产生。 此外,研究人员已经提出AAC可以介导线粒体解偶联,但人们难以证明该功能或阐明其机制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#转运#
42
#载体#
51
#Nat#
31
#ATP#
46
学习了,长知识
76