关节镜清理联合抗生素骨水泥链珠植入治疗前交叉韧带重建术后感染1例
2020-03-23 陶海兵 余昆 刘欣伟 创伤与急危重病医学
目前,关节镜下前交叉韧带重建术已成为治疗前交叉韧带损伤主要治疗方案。随着关节镜手术的普及,前交叉韧带重建术手术量的增加,术后疼痛、关节强直、感染等并发症发生率也逐渐升高。
目前,关节镜下前交叉韧带重建术已成为治疗前交叉韧带损伤主要治疗方案。随着关节镜手术的普及,前交叉韧带重建术手术量的增加,术后疼痛、关节强直、感染等并发症发生率也逐渐升高。其中,关节感染是关节镜手术较为严重的并发症。有研究报道,前交叉韧带重建术后感染发生率为0.84%;另一针对关节镜下前交叉韧带重建术后并发症的回顾性分析显示,0.25%的前交叉韧带重建术后出现感染。总体而言,前交叉韧带重建术后感染的发生率为0.14%~1.70%。若不能及时控制感染,会导致关节粘连强直、关节软骨丢失、慢性骨髓炎等严重后果。本研究采用关节镜清理联合抗生素骨水泥链珠植入治疗前交叉韧带重建术后感染1例,取得较好疗效,现报道如下。
临床资料
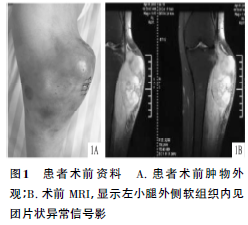
患者男性,30岁,于2018年4月因“左膝前交叉韧带损伤”行左膝关节镜下自体肌腱移植前交叉韧带重建术。术后第4天出现左膝关节肿痛,浮髌试验阳性,屈伸活动受限,髌上囊、关节间隙压痛,伴全身发热,体温最高达39.5℃。实验室检查结果显示,白细胞计数、中性粒细胞计数、红细胞沉降率、C反应蛋白、白细胞介素6均显著升高。关节穿刺液浑浊,呈黄褐色;关节液镜检白细胞满视野;细菌培养为鲍曼不动杆菌。患者明确关节感染诊断后,于2018年4月28日行关节镜清理、移植物取出、关节腔置管灌注冲洗引流术,术后仍反复发热,症状未见改善。遂于2018年5月28日,患者于北部战区总医院入院治疗。入院查体显示,体温38.6℃,脉搏81次/min,呼吸20次/min,血压132/80mmHg(1mmHg=0.133kPa),体质量72kg;左膝关节明显肿胀,皮温增高,浮髌试验阳性,髌上囊及关节间隙压痛阳性,左膝关节活动度70°-0°-0°。实验室检查结果:血红蛋白101g/L、白蛋白33.9g/L、白细胞计数10×109个/L、中性粒细胞计数7.1×109个/L、红细胞沉降率31mm/h、C反应蛋白48.9mg/L、白细胞介素69.3pg/ml。行关节穿刺,关节液行细菌培养(需氧菌培养、厌氧菌培养和真菌培养)及药敏试验。培养结果显示,鲍曼不动杆菌生长,对左氧氟沙星、替加环素、亚胺培南等药物敏感。结合临床表现及细菌培养结果,明确诊断为关节感染。
治疗方法
手术方法 患者行关节镜清理联合抗生素骨水泥链珠植入。全身麻醉后,术中见髌上囊、内外侧关节间隙、髁间窝及髌前滑膜增生、明显充血,髁间滑膜皱襞形成,弥漫性脓性分泌物及脓苔形成,关节囊弥漫充血,呈鲜红色,髌前脂肪增生,表面附有脓苔样物质,股骨髁、滑车关节、胫骨平台软骨表面及内外侧半月板呈炎性侵蚀样改变,前交叉韧带缺如,后交叉韧带呈糜烂样改变,弹性欠佳。关节镜下探查,见股骨、胫骨隧道表面骨质被侵蚀,隧道径口扩大,内植物已取出。明确病变后,关节镜下取病变滑膜组织作病理检查,彻底清理可见坏死组织、脓苔样组织、增生炎性充血滑膜组织及滑膜皱襞。利用射频消融进一步清理糜烂腐蚀的半月板、韧带组织及软骨。清理完毕后,反复检查关节内是否残余感染组织,术区仔细止血,使用双氧水及大量生理盐水反复冲洗整个关节囊及骨髓道,并使用Ⅲ型安尔碘盥洗整个关节囊并浸润关节腔约5min,而后再次大量生理盐水脉冲冲洗关节腔,直至关节液呈淡红色。根据术前药敏培养结果及经验,使用万古霉素及替加环素与骨水泥混合制作抗生素骨水泥链珠,将两串链珠并列从胫骨隧道导入,股骨隧道导出,牵引下自股骨外髁处顺利翻转Endobutton钢板,悬吊占位器链珠于股骨端,胫骨隧道多余部分剪除。再次冲洗关节腔并吸净残留液体,查无活动性出血,膝关节留置负压引流瓶,逐层缝合各层组织,无菌纱布包扎。见图1~3。
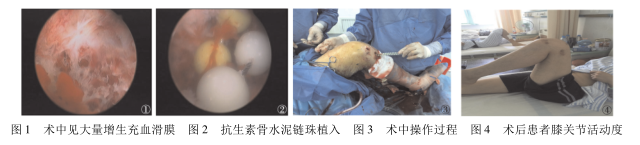
术后治疗与康复训练 结合药敏结果及临床药师会诊意见,每6h给予头孢哌酮舒巴坦3g/次、左氧氟沙星0.5g1次/d静脉滴注抗感染治疗;积极纠正贫血及低蛋白血症,适度抗凝预防下肢深静脉血栓,术后膝关节功能性支具伸直位固定。麻醉过后即开始肌力训练,以直腿抬高训练及踝泵功能训练加强股四头肌肌肉力量,术后早期患肢暂不负重,每隔3d复查炎性指标。经治疗后,患者体温次日降至38.0℃以下,1周后恢复正常;患肢关节肿胀明显消退,皮温下降,术后14d复查外周血白细胞计数、C反应蛋白、红细胞沉降率、白细胞介素6均回至正常水平。待实验室检查结果维持正常5d以上,关节液培养连续3次阴性后,停用静脉抗生素,改用口服抗生素治疗2周。出院时,患者可主动屈伸患膝关节,屈膝角度达110°,切口愈合良好,感染治愈。见图4。
讨论
前交叉韧带重建手术后感染后果严重,若诊治不及时、不确切将导致移植肌腱溶解、骨道扩大重建前交叉韧带失败、关节纤维化、感染扩散发生骨髓炎等严重后果。前交叉韧带重建术后感染一旦确诊,应及时进行关节镜清理手术,可保留移植物,提高疗效。本例患者感染致病菌为鲍曼不动杆菌,是近年来院内感染出现率较高的病菌,污染的医疗器械及侵入性操作是其主要传播媒介,极易对消毒剂和抗菌药物产生耐药性,且通常毒力较强。若单纯应用静脉抗生素或关节镜清创联合灌注冲洗治疗,见效缓慢,病情反复,常导致感染迁延不愈,且长期静脉滴注抗生素易导致耐药菌产生。而单纯灌注冲洗的患者需长期卧床,影响术后功能康复,增加外源性感染发生率。采用关节镜清理联合应用抗生素骨水泥链珠植入术治疗前交叉韧带重建术后关节内感染,不仅能清理关节腔内的脓性分泌物及被侵蚀的软组织,还能有效利用抗生素骨水泥链珠直接作用于关节内细菌,抑制繁殖。前交叉韧带重建术后感染常累及股骨及胫骨隧道,抗生素骨水泥链珠植入股骨及胫骨隧道中,抗生素直接在骨髓道中持续释放,使隧道局部抗生素药物浓度远高于其他给药途径,有效消除病灶。本例患者经治疗后,切口愈合良好,未出现流脓等症状,未再见体温持续升高,复查炎性指标均正常,关节活动度增加,贫血及营养不良等症状均明显改善。
综上所述,关节镜清理联合应用抗生素骨水泥链珠植入术可有效消除病灶,避免关节内结构持续受到侵蚀,控制骨髓炎发生,减少感染复发及手术次数,减轻患者经济负担,缩短静脉应用抗生素时间,避免耐药及因药物引起的肝、肾功能损害。
原始出处:
陶海兵,余昆,刘欣伟,刘松波,王宇,项良碧.关节镜清理联合抗生素骨水泥链珠植入治疗前交叉韧带重建术后感染1例[J].创伤与急危重病医学,2020,8(01):67-68.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#植入治疗#
41
#韧带重建术#
53
#骨水泥#
45
#关节镜#
49
#前交叉韧带#
47
#韧带#
45
#植入#
30