J Hypertens:儿童和青少年种族和动脉僵硬度之间的相关性分析!
2017-07-11 xing.T MedSci原创
由此可见,该研究的结果表明黑人青春期高cf-PWV值较高,独立于血压值。因此,该研究的数据表明青春期是成人黑人血管轮廓出现的关键阶段。
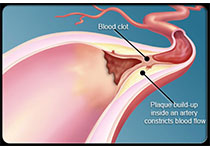
大动脉僵硬度增加是心血管疾病风险的重要决定因素。非洲裔美国人比成年白人相比具有更高的由颈股动脉脉搏波速度(cf-PWV)测得的动脉僵硬度。而评估儿童和青少年cf-PWV种族差异的研究较为稀缺。近日,高血压领域权威杂志Journal of Hypertension上发表了一篇研究文章,该研究旨在探讨儿童和青少年中种族与cf-PWV之间的相关性。
研究人员纳入了七百七十一名儿童和青少年(211名黑人和560名黑人,11.3±2.7岁)。采用cf-PWV评估了动脉僵硬度。民族分类是由一名采访者根据一般的表型,如肤色、头发形状和面部痕迹,来判断获得。
研究人员发现在青春期阶段在所有黑人和非黑人的血压是相似的。不同的是,黑人cf-PWV高于非黑人,在青春期(5.9±0.7 vs. 5.6±0.8米/秒,P=0.001)和青春期后(6.1±0.7 vs. 5.7±0.7米/秒,P=0.042),而在黑人和非黑人青春期阶段没有检测到差异。这些分析调整了性别、年龄、身高、体重指数、收缩压和心率。
由此可见,该研究的结果表明黑人青春期高cf-PWV值较高,独立于血压值。因此,该研究的数据表明青春期是成人黑人血管轮廓出现的关键阶段。
原始出处:
Zaniqueli, Divanei,et al. Ethnicity and arterial stiffness in children and adolescents from a Brazilian population.Journal of Hypertension. 2017. http://journals.lww.com/jhypertension/Abstract/publishahead/Ethnicity_and_arterial_stiffness_in_children_and.97676.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#儿童和青少年#
28
#TENS#
26
#相关性#
26
#PE#
30
#相关性分析#
31
#动脉僵硬#
35
#动脉僵硬度#
30
学习一下知识了
0